The EMRA Diversity & Inclusion Committee is proud to present "Why History Matters," a series that highlights leaders and events that illuminate the importance of diversity, equity, and inclusion in the field of medicine. In this installment we celebrate Henrietta Lacks.
In honor of Women's History Month, we chose to highlight Ms. Henrietta Lacks.
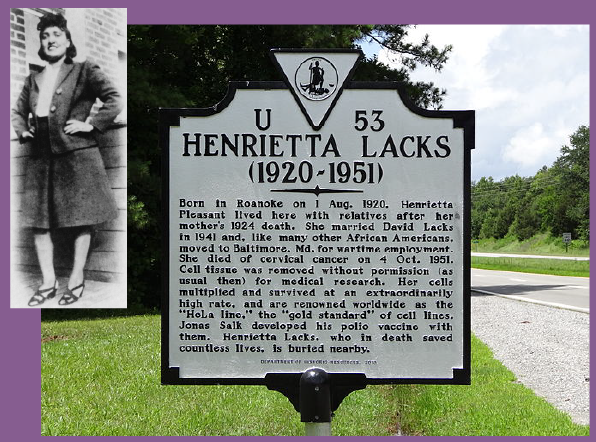
Ms. Lacks was an African-American woman born in 1920, whose cancer cells were taken without her knowledge and utilized to isolate immortal cell lines (HeLa cells) for biomedical research. Her cells served as the earliest and most commonly used human cell line in scientific research.
To this day, the HeLa cells are used to advance biomedical studies in numerous areas such as cancer research, virology and vaccine development, and even space biology. There are an estimated 11,000 patents involving HeLa cells. Controversy arose in the early 70s, nearly 25 years after Ms. Lacks' death, as these cells were still being utilized by researchers without family knowledge or consent.
May Ms. Lacks rest in peace knowing her life, legacy, and cells have continued to impact and advance the fields of medical and science.
To learn more, visit: https://pmc.ncbi.nlm.nih.gov/articles/PMC3516052/