Five Reasons Early-Career Emergency Physicians Should Consider Practicing in a Rural ED
By Leon C. Adelman, MD, MBA, FACEP
On a recent emergency department shift in rural central North Carolina, the charge nurse tapped me on the shoulder and said, “A 39-week pregnant patient just came through triage. Looks like she’s in labor.”
Walking toward the patient’s room, I asked the charge nurse to call OB. Her response: “Doctor, you are OB.” After thinking for a second, I asked her to call peds. She chuckled and said, “Doctor, you are peds.”
Having worked in rural EDs for the past five years, including two stints as a medical director, I have experienced many good reasons to practice rural emergency medicine. This article highlights five.
1. Master your craft
When thinking about a prospective job, have you thought, “Will this position help me improve my emergency medicine capabilities?” If so, rural EM is for you.
In a rural ED, nearly all procedures outside of an operating room are the emergency physician’s responsibility. Reducing fractures and dislocations while managing the procedural sedation? Check. Lateral canthotomy after an industrial accident? Check. Pediatric burr hole? Check!1
Dr. Glaucomflecken (Will Flanary) hilariously captures the broad skillset of the rural EM physician in his video, “First Day of Rural Medicine.”
2. Make more money
The Physicians Thrive 2022 Physician Compensation Report2 sums it up nicely: “Rural and underserved areas pay the highest salaries and the biggest bonuses.” Exact numbers are difficult to obtain, though a Merritt Hawkins report showed that job offers to family physicians in rural locations were on average 7.5% larger than the national average.3
WalletHub rankings showed an inverse correlation between a state’s population density and higher physician wages (adjusted for cost of living). The top five states for physician compensation were South Dakota, Indiana, Wisconsin, Mississippi, and Kentucky.4 A Healthcare Finance article explained, “Rural facilities tend to pay physicians more due to the difficulty in recruiting new talent to rural communities.”5
3. Rural EDs need you
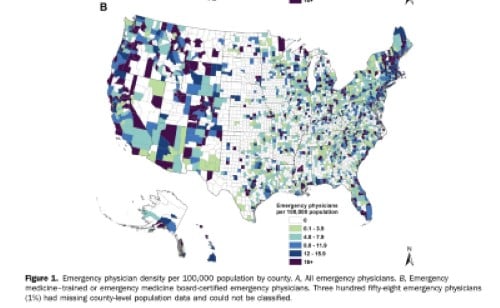
ACEP’s National Study of the Emergency Physician Workforce, 2020, quantified where U.S. emergency physicians live.6The authors found that only 8% of emergency physicians live in rural areas, compared with 15% of the general population. The article includes the following graphic showing dramatic differences in physician density across the country, mostly determined by regions’ level of urbanization.
The undersupply of emergency physicians in rural areas is worsening with time. A 2022 study of U.S. emergency physicians found “a concerning trend regarding the recruitment of rural emergency physicians. From 2013 to 2019, the number of emergency physicians entering the rural workforce never offset the number leaving from the prior year, suggesting that shortages and inequities in access will persist unless substantial efforts are made to address emergency physician recruitment and retention issues.”7
4. Rural ED patients need you
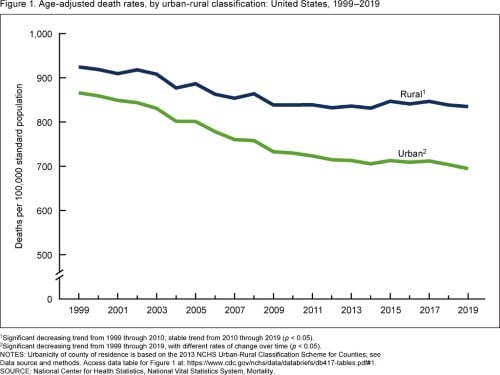
Generally, health outcomes in rural parts of the United States are worse than in urban regions. A CDC MMWR article summarizes, “Rural communities experience higher age-adjusted death rates and a higher number of potentially excess deaths from the five leading causes compared with urban areas. Higher death rates and potentially excess deaths are often associated with various interconnected societal, geographic, behavioral, and structural factors.”8
The gap between urban and rural health outcomes is widening. A 2021 National Center for Health Statistics report9includes the following chart of pre-COVID data:
5. Rural patients will be grateful for your work
In my experience, patients in rural EDs tend to have patience for systemic imperfections and plenty of gratitude for the work emergency clinicians do on their behalf.
When I entered the room of the pregnant patient in labor at our rural ED, she noticed that our crew was far from a well-oiled baby-delivering machine. For example, we did not have a proper pelvic bed. She looked at me and asked, “Do you deliver many babies here?” I honestly responded, “Once in a while.” Apparently, that was enough reassurance. She trusted us, and we delivered a healthy, beautiful baby girl to a healthy, grateful new mom.
Leon C. Adelman, MD, MBA, FACEP, is co-founder and CEO of Ivy Clinicians.
References
- Rural Medicine: Cranial Burr Hole. In: EM:RAP [Internet]. [cited 2 Aug 2022]. Available: https://www.emrap.org/episode/emrap2021/ruralmedicine
- Physician Thrive’s Physician Compensation Report [2022 Report]. In: Physicians Thrive [Internet]. 22 Jan 2022 [cited 2 Aug 2022]. Available: https://physiciansthrive.com/physician-compensation/report/
- [No title]. [cited 2 Aug 2022]. Available: https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/mha_whitepaper_rural_PDF.pdf
- Kiernan JS. Best & Worst States for Doctors. In: WalletHub [Internet]. 21 Mar 2022 [cited 2 Aug 2022]. Available: https://wallethub.com/edu/best-and-worst-states-for-doctors/11376
- Lagasse J. Physician compensation at Midwest rural hospitals is higher than the national average. In: Healthcare Finance News [Internet]. [cited 2 Aug 2022]. Available: https://www.healthcarefinancenews.com/news/physician-compensation-midwest-rural-hospitals-higher-national-average
- Bennett CL, Sullivan AF, Ginde AA, Rogers J, Espinola JA, Clay CE, et al. National Study of the Emergency Physician Workforce, 2020. Annals of Emergency Medicine. 2020. pp. 695–708. doi:10.1016/j.annemergmed.2020.06.039
- Gettel CJ, Courtney DM, Janke AT, Rothenberg C, Mills AM, Sun W, et al. The 2013 to 2019 Emergency Medicine Workforce: Clinician Entry and Attrition Across the US Geography. Ann Emerg Med. 2022. doi:10.1016/j.annemergmed.2022.04.031
- Garcia MC. Reducing Potentially Excess Deaths from the Five Leading Causes of Death in the Rural United States. MMWR Surveill Summ. 2017;66. doi:10.15585/mmwr.ss6602a1
- Products - Data Briefs - Number 417 - September 2021. 20 Sep 2021 [cited 2 Aug 2022]. doi:10.15620/cdc:109049
Image Credits
Figure 1, Emergency physician density by 100,000 population by county. Image Source: Bennett CL, Sullivan AF, Ginde AA, et al. National Study of the Emergency Physician Workforce, 2020. Annals of Emergency Medicine. December 2020;76(6):794.
Figure 1, Age-adjusted death rates, by urban-rural classification: United States, 1999-2019. Image Source: Curtin SC, Spencer MR. Trends in Death Rates in Urban and Rural Areas: United States, 1999-2019. U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics, National Vital Statistics System, Mortality. NCHS Data Brief, No. 417. September 2021. NCHS reports can be downloaded here.
Related Content


Jan 13, 2023
The 5 Best Resources for Navigating the Community Emergency Medicine Job Market
With the abundance of job search options and generic job sites like Indeed and ZipRecruiter, it’s easy to feel overwhelmed when trying to decide which resource to use. EMRA asked Dr. Leon Adelman, co-founder and CEO of Ivy Clinicians, about available job search options — and the upsides and downsides of each — for residents specifically as they plan their post-residency careers in EM. Here’s Dr. Adelman’s advice.




