What is Disaster Medicine? An Interview with Natalie Moore, MD, MPH
Brock Chimileski, MSII, University of Connecticut School of Medicine
The field of disaster medicine provides exciting and challenging opportunities to travel the globe and assist some of the most vulnerable communities after major catastrophes. To learn more about it, we spoke with Dr. Natalie Moore, an emergency physician and the first graduate of the new International Disaster Medicine Fellowship program at the University of Connecticut (UConn).
What is the physician’s role in disaster response?
“Whatever roles need to be filled!”
Dr. Moore explains that each deployment comes with unique opportunities and challenges. Typically, a physician will register with an organization, whether governmental or nongovernmental, that manages the recruitment of interdisciplinary response teams when a natural or man-made disaster occurs. Dr. Moore personally volunteers with International Medical Corps, and throughout her early career she has assisted in the Caribbean, Africa, and the Middle East during hurricane responses, for refugee camp aid, and more. In these settings, she has helped construct and operate field hospitals, staffed overpopulated EDs, traveled by RV to isolated communities as part of mobile medical units, as well as providing more standard outpatient care. Above all, she emphasizes the importance of strong communication with the community to properly address their specific needs, advocate for the allocation of resources, and develop sustainable initiatives that can be continued by the communities once they regain their strength and the response team returns home. No matter what, all positions require flexibility and open-mindedness, leadership, and learning how to become comfortable in not-so-comfortable situations.
What interests you about disaster medicine?
“The necessity of quickly adapting to frequently changing conditions and challenges, the utilization of a skillset much wider than medicine alone, and, of course, providing tangible aid for exceptionally vulnerable communities in need.”
Dr. Moore had early experience as an EMS provider which led her towards specializing in EM. As a third-year medical student, she had the opportunity to work at St. Jude’s Hospital on the island of St. Lucia, in the West Indies; a low resource setting. Dr. Moore was inspired by how this environment required her to rely much more heavily on her clinical reasoning skills rather than depending on lab tests and imaging. She found an esteemed mentor in the field, Dr. Robert Fuller at UConn, continued her training in EM, and then became the first fellow of UConn’s International Disaster Medicine Fellowship after finishing her residency at Baystate Medical Center in Massachusetts. She is now an attending physician at UConn Health’s John Dempsey Hospital and continues to work frequently in disaster response.
What changes have happened to the field of disaster medicine recently?
“There is more recognition and emphasis on evidence-based practice and standardization, aimed at improving accountability and quality of care.”
Although disaster relief has always been a part of medicine, it has undergone significant professionalization in recent decades. Dr. Moore gives a few examples: more stringent credentialing standards for relief organizations and providers, the Cluster System created by the United Nations Inter-Agency Standing Committee, and The Sphere Project created by a large team of international humanitarian professionals. The Cluster System improves coordination and the division of labor between multiple groups responding to humanitarian emergencies to reduce the duplication of services and promote better allocation of resources, and The Sphere Project has developed a distinct set of principles and guidelines that all relief organizations are expected to follow to create a higher standard of care. Through these examples and more, there have been major advances in accountability, organization, and quality of care provided by all medical-humanitarian response efforts.
Why are disaster medicine fellowships important?
“Dedicated, protected time for developing the skills and experiences needed to be a leader in the field.”
There are about ten disaster medicine fellowship programs across the United States, with several recently receiving SAEM approval. Dr. Moore values her fellowship training because she believes it allowed her to jump start her career in global medicine in a way that wouldn’t have been possible if she went straight into a position as an attending physician. UConn’s program includes didactic labs that provide formal preparation to handle many of the disaster management logistics that new learners may initially overlook, like camp setup and hygiene, basic plumbing and electrical work, and more. She also appreciated UConn’s combined MPH program (a common feature for Disaster Medicine Fellowships), because that provided extra initiative to work on related projects of interest. Overall, the program gave her ample opportunity to travel, network, and learn directly from mentors in the field.
What opportunities exist for interested medical students?
“Many! Your specific school may provide the best opportunity to travel as a student, but it is worthwhile to start looking into national organizations as well.”
There are ways to get involved at a local and a national level, though some national programs have restrictions for students. For specific service trips, look into your school’s opportunities, as these often provide the best chance for students to travel. Peruse your school website and/or ask around your EM interest group or your department’s emergency physicians. In addition to what your school offers, great places to start learning about more national opportunities are EMRA’s Prehospital and Disaster Medicine Committee and ACEP’s Disaster Medicine page. These do a great job at providing information about disaster medicine in general as well as providing links to further resources.
Related Content

Jun 25, 2020
Program Director Interview Series: Radosveta Wells, MD | EM Residency Program Director at Texas Tech University Health Sciences Center El Paso, El Paso, TX
In this installment of the Program Director Interview Series we sit down with Radosveta Wells, MD to learn about the EM Residency at Texas Tech University Health Sciences Center El Paso.
Jun 11, 2020
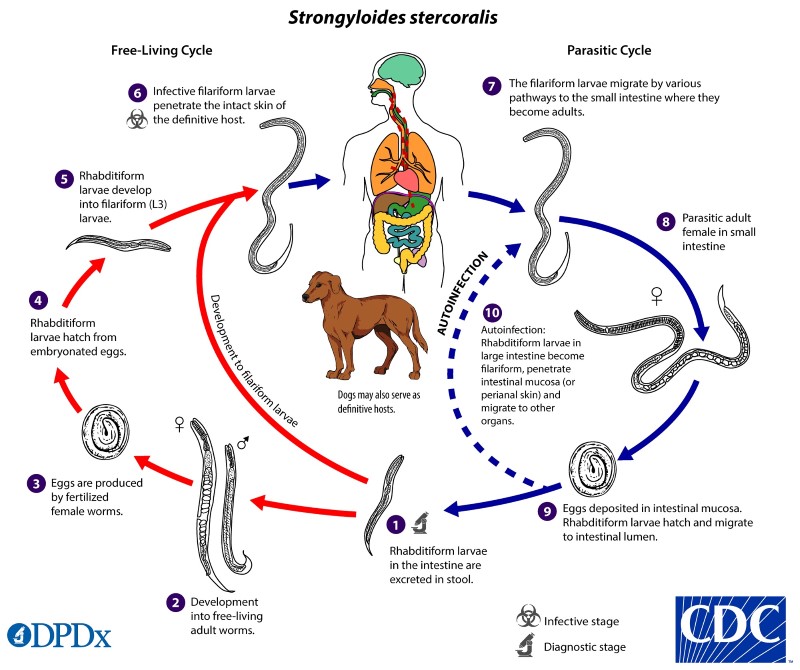
A Pause to Consider Strongyloides Stercoralis in the ED
Strongyloidiasis is an infection of the parasitic nematode, Strongyloides stercoralis. This condition is well-known in global health as a concern among immigrants and refugees, but it is also present in many rural areas of the United States. What treatments should be considered or avoided when providing emergency care for patients at risk for this condition?





