Two EKG Patterns You Must Know Before Your EM Rotation: Wellens and Brugada
Allison Gasnick, MS4
Case Western Reserve University School of Medicine
Medical Student Council Editor 2024-2025
Edited by:
Jeremy Berberian, MD
EM Resident ECG Challenge Faculty Editor
EMRA EKG Guide Editor-in-Chief
Associate Director of Resident Education, Department of Emergency Medicine, Christiana Care Health System
Two syndromes, Wellens' Syndrome and Brugada Syndrome, have distinct EKG patterns that are essential for providers, including medical students, to recognize. This article provides an overview of the EKG findings for these syndromes, aiding in their identification and understanding.
Wellens' Syndrome
Wellens' Syndrome is a pattern of EKG changes indicating a critical stenosis of the proximal left anterior descending (LAD) artery. It suggests high likelihood of developing anterior myocardial infarction (MI). Recognizing Wellens' Syndrome is crucial as the patients require admission for cardiac catheterization.
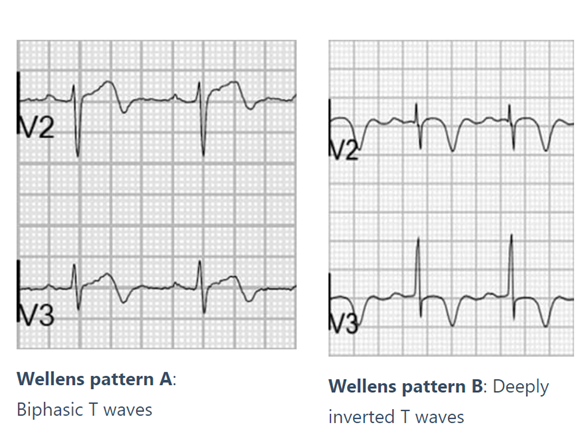
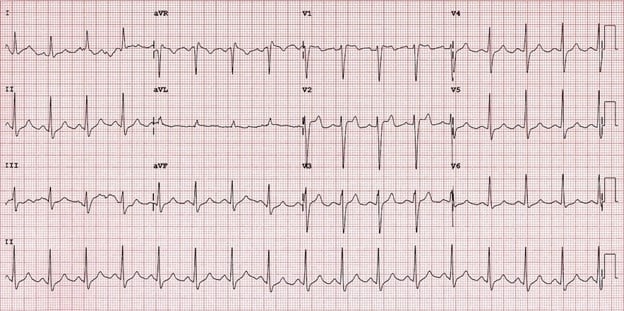
Wellens' Syndrome is characterized by specific EKG changes in the precordial leads (typically leads V2 and V3) that are thought to represent reperfusion after an ischemic event. These changes occur in the context of recent, but resolved, chest pain and often normal or minimally elevated cardiac enzymes. There are two types of Wellens' EKG patterns:
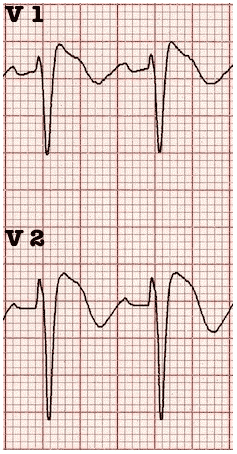
Type A (25% of cases): Biphasic T waves, typically in leads V2 and V3. The initial portion of the T wave is positive, followed by a deep negative deflection.
Type B (75% of cases): Deeply inverted, symmetric T waves, typically in leads V2 and V3.
Diagnostic Criteria
- Deeply inverted or biphasic T waves in V2-3 (may extend to V1-6)
- EKG pattern present in pain-free state
- Isoelectric or minimally-elevated ST segment (< 1mm)
- No precordial Q waves
- Preserved precordial R-wave progression
- Recent history of angina
- Normal or slightly elevated serum cardiac markers
T-wave Evolution
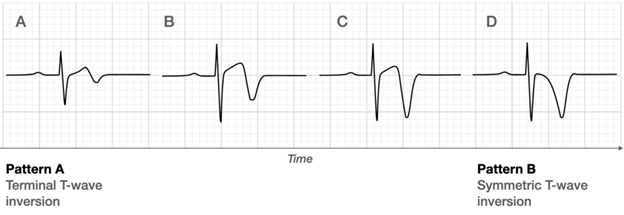
Clinical Significance of the T-wave Evolution
A sudden complete occlusion of the LAD results in a transient anterior MI, causing anginal symptoms such as chest pain and diaphoresis. Reperfusion of the LAD leads to cessation of anginal symptoms and improvement/resolution of ST elevations, and the development of biphasic or inverted T waves. If the artery stays open, these T waves gradually evolve from biphasic to deeply inverted, resulting in the T wave evolution depicted above. However, coronary perfusion remains unstable due to severe stenosis and the risk for re-occlusion remains high. If re-occlusion occurs, the first EKG sign is pseudo-normalization of the T waves, which describes when inverted T-waves become upright and prominent hyperacute T-waves indicating ischemia and an impending MI. These EKG changes will be accompanied by a return of anginal symptoms, although the EKG changes can sometimes precede the symptoms. In these cases, the patients should be taken to the cardiac catheterization lab emergently for coronary angiography and possible PCI. For the patients that remain symptom free with EKG changes consistent with Wellens’ syndrome, admission for urgent cardiac catheterization is appropriate.
Brugada Syndrome
Brugada Syndrome is a genetic condition associated with an increased risk of sudden cardiac death due to fatal arrhythmias. It is caused by mutations affecting cardiac sodium channels, leading to characteristic EKG changes and a predisposition for unprovoked dysrhythmias such as ventricular fibrillation or polymorphic ventricular tachycardia. The diagnostic criteria include both clinical criteria and EKG changes.
Clinical Criteria
To make the diagnosis, the EKG changes must be associated with any one of the following clinical criteria:
- Documented ventricular fibrillation (VF) or polymorphic ventricular tachycardia (VT)
- Family history of sudden cardiac death at <45 years old
- Coved-type EKGs in family members
- Inducibility of VT with programmed electrical stimulation
- Syncope
- Nocturnal agonal respiration
EKG Findings
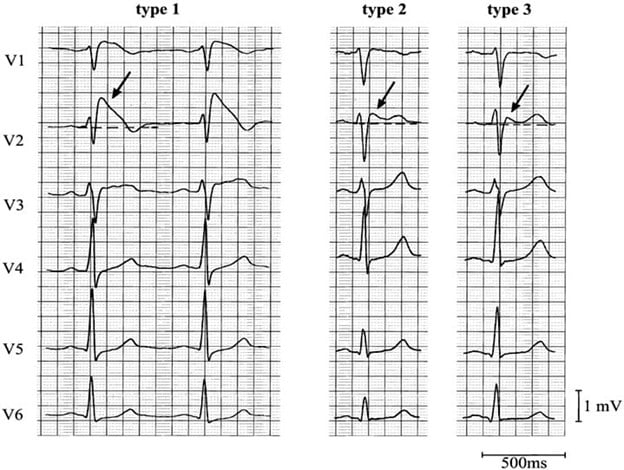
The EKG changes seen with Brugada Syndrome occur in the right precordial leads (V1-V3) and are classified into three types:
Type 1: Coved-type ST-segment elevation ≥2 mm in >1 of V1-V3 followed by a negative T wave. This pattern is considered diagnostic of Brugada Syndrome.
Type 2: Saddleback-shaped ST-segment elevation ≥2 mm. This morphology is no longer considered diagnostic but may warrant further testing in the appropriate clinical scenario.
Type 3: Type 1 or 2 morphology with < 2mm ST-segment elevation. This morphology is non-diagnostic.
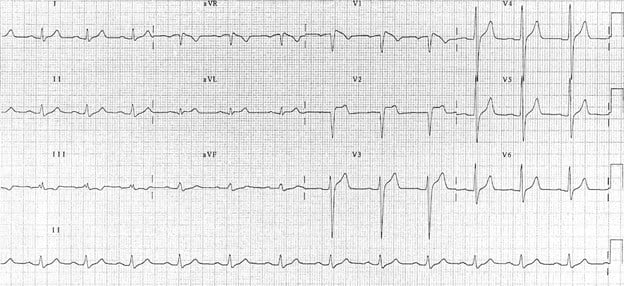
Clinical Significance
Patients with Brugada Syndrome are at risk for sudden cardiac arrest, particularly during sleep or rest. The condition is often unmasked by fever, certain medications, or electrolyte imbalances. Diagnosis is confirmed through EKG findings and genetic testing. Definitive treatment for symptomatic patients is placement of an implantable cardiac defibrillator.
Recognition and Management
Understanding the EKG findings of Wellens' and Brugada Syndromes is crucial for timely diagnosis and management. Wellens' Syndrome requires urgent coronary intervention to prevent a myocardial infarction, while Brugada Syndrome necessitates strategies to mitigate the risk of sudden cardiac death, including possible ICD placement.
Key Points
- Wellens' Syndrome:
- Seen in asymptomatic patients with recent history of anginal symptoms
- EKG changes represent reperfusion in the setting of a critical stenosis of the proximal LAD
- Look for biphasic or deeply inverted T waves in the precordial leads, typically V2 and V3
- Brugada Syndrome:
- Sodium channelopathy that can lead to sudden cardiac death from ventricular dysrhythmias
- Includes both clinical and EKG criteria
- Look for coved ST-segment elevations in leads V1-V3 in patients presenting with syncope
References
- Electrocardiogram in the diagnosis of myocardial ischemia and infarction - UpToDate. Accessed June 23, 2024. https://www.uptodate.com/contents/electrocardiogram-in-the-diagnosis-of-myocardial-ischemia-and-infarction?search=wellens%20syndrome&source=search_result&selectedTitle=1%7E4&usage_type=default&display_rank=1
- Wellens Syndrome • LITFL • ECG Library Eponym. Accessed June 23, 2024. https://litfl.com/wellens-syndrome-ecg-library/
- Miner B, Grigg WS, Hart EH. Wellens Syndrome. StatPearls. Published online July 31, 2023. Accessed June 23, 2024. https://www.ncbi.nlm.nih.gov/books/NBK482490/
- Brugada Syndrome: An ECG Pattern You Need to Know. Accessed June 23, 2024. https://www.aliem.com/brugada-syndrome-an-ecg-pattern-you-need-to-know/
- Mizusawa Y, Wilde AAM. Brugada syndrome. Circ Arrhythm Electrophysiol. 2012;5(3):606-616. doi:10.1161/CIRCEP.111.964577
- Sayed M El, Goyal A, Callahan AL. Brugada Syndrome. StatPearls. Published online August 8, 2023. Accessed June 23, 2024. https://www.ncbi.nlm.nih.gov/books/NBK519568/
- Brugada syndrome: Clinical presentation, diagnosis, and evaluation - UpToDate. Accessed June 23, 2024. https://www.uptodate.com/contents/brugada-syndrome-clinical-presentation-diagnosis-and-evaluation
Related Content

Aug 25, 2017
Your Home
The Emergency Medicine Residents' Association EMRA is the voice of emergency medicine physicians-in-training and the future of our specialty and the largest and oldest independent resident organization in the world. EMRA was founded in 1974 and today has a membership over 18,000 residents, medical students, and alumni.