Practicing Medicine In The Wilderness
Elizabeth Kleiner, MSIV, Des Moines University College of Osteopathic Medicine
EMRA MSC Great Plains Regional Representative 2019-20
Wilderness medicine is a subspecialty of EM that is typically defined as the practice of medicine in resource-poor, austere environments. Since it entails limited resources and harsh conditions, typically far away from the conveniences of modern medicine, it can be argued that Greek and Roman naval surgeons were likely the first people to practice wilderness medicine. Advancements in military and tactical medicine have always been closely linked to developments in wilderness medicine, and the two subspecialties continue to evolve and advance together.
Wilderness medicine as we know it today, however, originated formally in 1983 with the formation of the Wilderness Medicine Society (WMS). Co-founders Drs. Paul Auerbach – author of the reference book Medicine for the Outdoors: The Essential Guide to Emergency Medical Procedures and First Aid – Ken Kizer, and Ed Geehr formed the WMS with the specific aim “to encourage, foster, support, and conduct activities or programs concerned with life sciences which may improve the scientific knowledge of the membership and the general public in matters related to wilderness environments and human activities in these environments.” The first subspecialty fellowship was established in 2003 at Stanford University Medical Center by Dr. Eric A Weiss.
The breadth of wilderness medicine cannot be overstated. It ranges from initial triage and evacuation of injured hikers and climbers to providing care for illness and injuries sustained by a group over the course of an expedition. Wilderness medicine is not just a fringe field in emergency medicine; it necessitates a profound understanding of the usefulness of clinical assessment and interventions. You must maximize efficiency of time and physical resources in the context of a resource-poor environment. Wilderness medicine providers are trained to improvise with what they have on hand, emphasizing multi- and cross-functionality. Prioritizing multi-functionality means carrying items that can be used for multiple purposes, such as IV start kits for IVs as well as needle cricothyroidotomy. Cross-functionality involves using items for different tasks in the event that the item created for that specific task is not available. For example, plastic bags used in place of gloves.
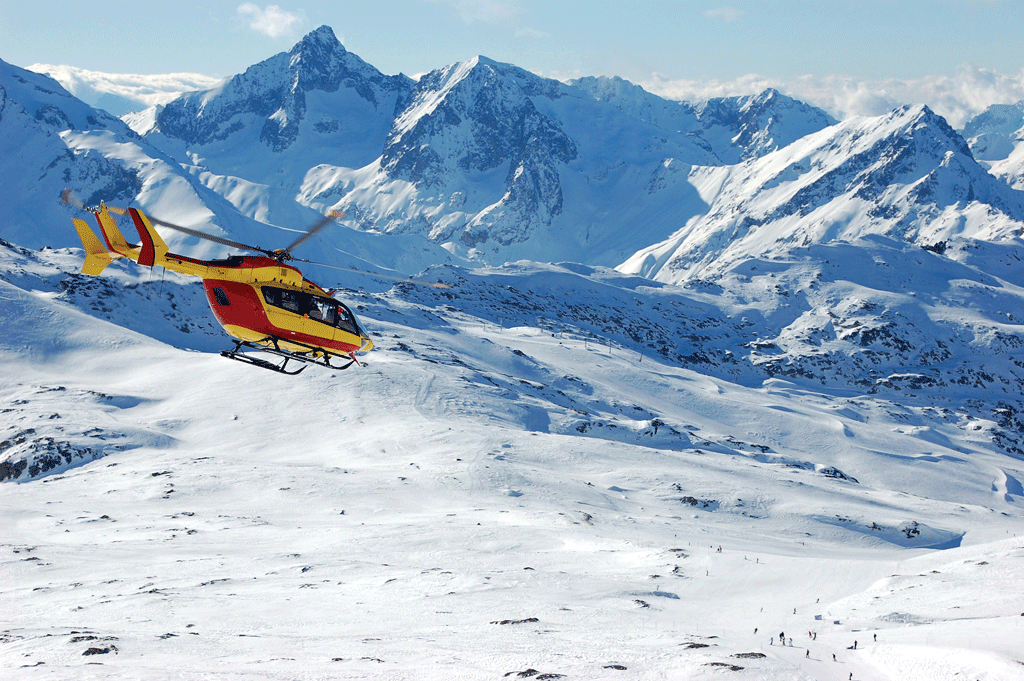
Within wilderness medicine there are a wide range of domains of specialist knowledge and training to explore, including rescue and evacuation, hyperbaric medicine, tropical medicine, disaster medicine, high-altitude medicine, and expedition and survival medicine. So what opportunities are available within this subspecialty?
What does the role of a wilderness medicine physician look like?
There are many reasons to pursue wilderness medicine and, depending on your interests, your role can look very different. If you are interested in expedition medicine, you may have the opportunity to accompany a group on a trek that requires or encourages that group to bring a physician. Along the way you may treat snake bites, sprained ankles, heat exhaustion, hypothermia, etc. depending on where you are venturing. The role of the health care provider is to be able to treat what comes along with whatever resources they have on hand. Improvisation and creativity are key in this role – as well as a healthy interest in adventure. The possibilities with wilderness medicine are only limited by your imagination and how much effort you are willing to put in.
What training options are available for medical students?
For medical students, there are a number of wilderness medicine away rotations available through AAMC’s VSLO portal and on individual program websites. In addition, there are rotations with NASA in Aerospace Medicine and there are a number of unique rotations listed on the SAEM website. Other options for training include certifications such as Advanced Wilderness Life Support (AWLS), Wilderness First Responders (WFR), Wilderness EMT, Wilderness First Aid, Wilderness Advanced First Aid, and more. There are many opportunities across the globe to become trained in all things wilderness, but a good place to start to check out upcoming courses and certifications are NOLS and Advanced Wilderness Life Support websites.
What professional opportunities are available after residency?
If if you are interested in exploring fellowship programs, a formal list of fellowships can be found through the ACEP wilderness medicine section. None are currently ACGME accredited, as an ACGME accreditation for wilderness medicine fellowships does not currently exist. Additionally, a formal fellowship is not required to become established in wilderness medicine. Other information can be found in the EMRA Fellowship Guide and via the EMRA Wilderness Committee. If you are interested and would like to find a mentor in wilderness medicine, please sign up for a virtual mentor here.