PoCUS Pitfalls
Nick Gualtieri, OMS-III, 2nd Lt, USAF, Ohio University Heritage College of Medicine
Rich Dowd, OMS-IV, Ohio University Heritage College of Medicine
EMRA MSC Midwest Coordinator
Samuel Southgate, MD, PGY-1, Regions Hospital, Saint Paul, Minnesota
EMRA Ultrasound Committee Chair-elect
Point of care ultrasound (PoCUS) is an increasingly used tool in the EM physician’s diagnostic arsenal. In fact, the Accreditation Council for Graduate Medical Education (ACGME) has listed it as a core competency for graduating EM physicians. Ultrasound, just like physical examination and other clinical skills, is a set of techniques that requires practice; there is no substitute for simply getting your hands on the probe and practicing. However, relative to basic clinical skills, there is wide variability between medical schools in the amount of formal ultrasound instruction students receive. As a result, there is wide variability in the baseline ultrasound knowledge and skill levels among rising EM interns. This article is not meant to teach the basics of ultrasound as this information is extensively covered throughout the FOAMed world (we like 5 Minute Sono). Instead, we aim to identify some of the most common pitfalls encountered by novice ultrasonographers and how to avoid them.
Exam: Echocardiography
Point-of-care echocardiography provides rapid assessment of global cardiac function and cardiac pathology.
- Pitfall: Distinguishing pericardial effusion and pleural effusion
Regardless of anatomic location, fluid appears hypoechoic on ultrasound. When using echocardiography to evaluate for the presence of pericardial effusion, it is critical that the location of the hypoechoic fluid is accurately interpreted--a common challenge for new ultrasound users. Is the fluid contained within the pericardium? Or is it within the pleural space? Fortunately, there is an anatomical landmark that can help a new user feel more certain of their interpretation: the descending thoracic aorta. The presence of fluid anterior to the descending aorta suggests a pericardial effusion (Figure 1), while fluid posterior to the descending aorta, likely represents a pleural effusion (Figure 2). Correctly identifying the location of pericardial/pleural fluid with ultrasound will expedite the patient’s diagnostic and treatment course, while failure to differentiate a pericardial effusion from a pleural effusion can result in unnecessary and unsuccessful pericardiocentesis.
Learn more about the role of PoCUS in diagnosing pericardial effusions here.
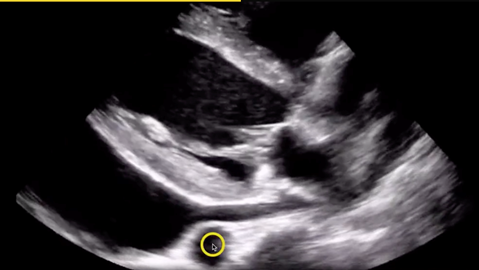
Figure 1. Pericardial effusion with descending aorta denoted by circle.
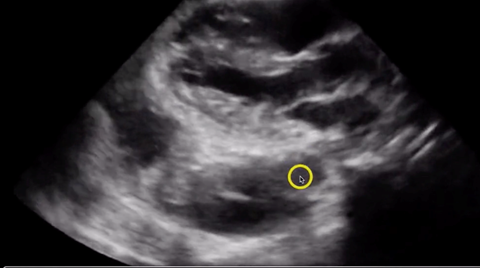
Figure 2. Pleural effusion with descending aorta denoted by circle.
Exam: FAST
The Focused Assessment with Sonography for Trauma (FAST) exam is a core skill for emergency physicians. Scanning the abdomen, pelvis and pericardium for free fluid allows us to assess for internal hemorrhage rapidly at the bedside. To ensure a thorough FAST exam, there are four areas we interrogate with ultrasound including: the right upper quadrant (RUQ), the left upper quadrant (LUQ), the pelvis, and the pericardial sac.
- Pitfall: Failing to visualize the caudal tip of the liver when evaluating Morison’s pouch
The RUQ view of Morison’s pouch (the hepatorenal recess) is the most sensitive element of the FAST exam for detecting intra-abdominal free fluid. However, one common pitfall is not scanning all the way through the liver to visualize the caudal tip. In fact, the caudal tip of the liver has been shown to be the most sensitive location for the evaluation of intra-abdominal free fluid within the RUQ scan.
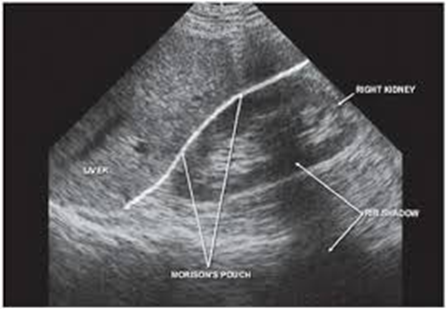
Figure 3. Morrison’s pouch.
In Figure 3, you will note the hepatorenal interface is absent of free fluid. Obtaining this initial view, without visualizing the caudal tip of the liver, and calling it a negative RUQ scan is a common mistake among novice scanners. By scanning through the liver to visualize the caudal tip, as in the GIF below, the user is able to detect a large pocket of free fluid that would have been missed had they stopped at simply visualizing the hepatorenal interface.
This is why you never call a RUQ FAST view negative unless you've seen the liver tip!#FOAMed pic.twitter.com/UZjcAMh32u
— Sam Ghali, M.D. (@EM_RESUS) March 27, 2017
Exam: Abdominal Aorta
We use ultrasound to assess the abdominal aorta for the presence of aneurysm. The normal diameter of the abdominal aorta is less than 3 cm.
- Pitfall: Failing to measure the aortic diameter from outer wall to outer wall
When measuring the aortic diameter with ultrasound, it is imperative to measure from the aorta’s outer wall to its contralateral outer wall. It is possible for clotted blood to occupy space within an aneurysm, causing the illusion that no aneurysm is present. The operator must be certain to measure the entire width of the aorta such that the true diameter of the aorta (including a potential aneurysm) is represented in the measurement. Figure 4 depicts an abdominal aortic aneurysm with clotted blood occupying much of the aneurysm. Ensure that your measurement includes the entire width of the aorta; you can see that this drastically alters the aortic diameter measurement from 2 cm to 7 cm, which completely changes the clinical picture associated with the measurement.
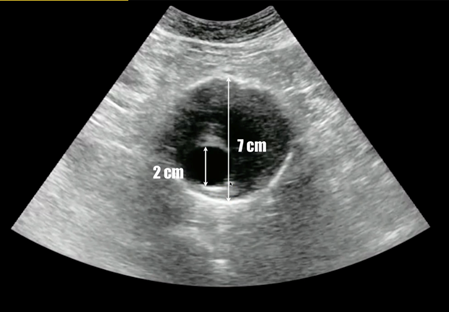
Figure 4. Abdominal aneurysm in cross section.
Exam: Lower extremity deep vein thrombosis
Evaluating patients for deep vein thrombosis (DVT) is a common task for emergency physicians. PoCUS allows us to scan the bilateral lower extremities, beginning proximally at the common femoral vein and compressing the vein in multiple locations to evaluate for presence of a clot (Figure 5).
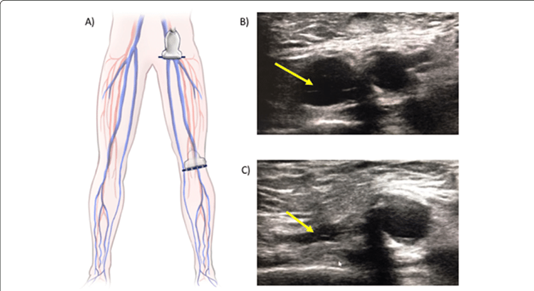
Figure 5. Sites of compression for two-point compression test for DVT.
- Pitfall: Inaccurate interpretation of venous compressibility
To confirm the absence of DVT, the scanner must observe complete collapse of the venous segment. When assessing venous compressibility, be sure that you visualize the venous walls making contact with each other, and that the venous lumen is entirely eliminated, as demonstrated in Figure 6. Inability to completely eliminate the venous lumen is suggestive of a clot - even if no thrombus is visualized - since early clots may appear anechoic as in Figure 7.
Figure 6. Complete collapse of the popliteal vein, the non-pulsatile vessel seen alongside the pulsatile popliteal artery, ruling out a DVT at this location.
Figure 7. No clot is visualized but the popliteal vein (the non-pulsatile vessel) fails to compress, suggesting a DVT.
In conclusion, point of care ultrasonography is an essential skill in every emergency physician’s diagnostic repertoire. It is a skill that is operator-dependent, so it is up to you to constantly look to improve both image acquisition and interpretation. While there is no substitute for deliberate hands-on practice, being aware of these common pitfalls will help you in your early days of scanning.
For more in-depth coverage of these topics, consider joining EMRA’s Ultrasound Committee.
References
- Accreditation Council for Graduate Medical Education 2020. ACGME Program Requirements for Graduate Medical Education in Emergency Medicine. Accessed 01 February 2021.
- Tarique U, Tang B, Singh M, Kulasegaram K, and Ailon J. (2018), Ultrasound Curricula in Undergraduate Medical Education: A Scoping Review. J Ultrasound Med. 2017 Jul; 37: 69-82.
- Core Ultrasound. Pericardial Effusion. Retrieved 30 January 2021 from https://www.coreultrasound.com/pericardial-effusion/. Screenshot by author.
- Lobo V, Hunter-Behrend M, Cullnan E, Higbee R, Phillips C, Williams S, Perera P, and Gharahbaghian L. Caudal Edge of the Liver in the Right Upper Quadrant (RUQ) View Is the Most Sensitive Area for Free Fluid on the FAST Exam. West J Emerg Med. 2017 Feb; 18(2):270-280. doi: 10.5811/westjem.2016.11.30435
- Radiology Key. Trauma. Retrieved 30 January 2021 from https://radiologykey.com/trauma-11/.
- Core Ultrasound. Aortic Aneurysm. Retrieved 30 January 2021 from https://www.coreultrasound.com/aaa/. Screenshot by author.
- Cid X, Canty D, Royse A, Maier A, Johnson D, El-Ansary D, Clarke-Errey S, Fazio T and Royse C. Impact of point-of-care ultrasound on the hospital length of stay for internal medicine inpatients with cardiopulmonary diagnosis at admission: study protocol of a randomized controlled trial—the IMFCU-1 (Internal Medicine Focused Clinical Ultrasound) study. Trials. 2020 Jan; 21, 53. https://doi.org/10.1186/s13063-019-4003-2
- Kopinski H and Davis L (sonographers). 2018. Negative Popliteal Vein Compression Test. [GIF]. https://www.thepocusatlas.com/soft-tissue-vascular
- Singh S (sonographer). Positive Popliteal Vein Compression Test. [GIF].
Related Content


Aug 17, 2022
Beginner's Guide to POCUS for Medical Students
Are you a medical student interested in point-of-care ultrasound? Don’t know where to start? The use of POCUS has grown significantly over the last few decades. It serves as a cost-effective tool for rapid, real-time assessment of a variety of pathology and helps guide decision making, such as administration of IV fluids based on IVC collapsibility. POCUS has also been shown to increase patient satisfaction and trust in the physician’s assessment. Without further ado, let’s delve into some steps you can take as a medical student to learn about POCUS!




