Transitioning from Medical Provider to Medical Student
Matthew Carvey MSIV, EMT-P, FP-C, TP-C - St. George’s University
EMRA MSC International Representative, 2021-2022
Medic-1 is responding to an assault in a rural location. Dispatch notifies EMS that the patient
has a fever and was put on mandatory self-isolation for 14 days. On arrival, EMS dons a sterile
cap, goggles, an N95 mask, face shield, gown and gloves. The patient, belligerent and
intoxicated on alcohol and psilocybin, yells at EMS ‘I have the COVID!’. She rushes EMS,
removes the practitioner’s mask, and coughs in his face. Police arrest the woman under the
Mental Health Act, and EMS transports, only for her to spit and verbally abuse them the entire
length of transport. EMS unloads the patient and awaits triage. One of the practitioners displays
signs of COVID-19 three days later. This case summarizes the all-too-familiar circumstances
many healthcare practitioners face while on the job. The primary purpose of this article is to
highlight the difficulties these previous providers have during medical school.
The COVID-19 pandemic has united the medical community – physicians, nurses, respiratory
therapy, and EMS (among many other examples) – in the singular purpose of containing the
virus. With this comradery comes shared challenges, such as fear of contracting the virus,
overwhelming PPE shortages and frontline staff burnout. Because of these concerns facing
society, a unique population of medical providers, as listed above, have taken on the trials of
becoming a medical student to pursue their vision of becoming a physician. This is not an easy
adjustment, with many challenges not typically found in your average student. Below are a few
of those issues that may arise, and some advice on how to deal with them.
- The difficulty of becoming a backseat driver in patient care after being the primary
provider. A major struggle of those with previous lead experience in medicine is that of
now becoming the one learning rather than doing. A way to overcome this is
remembering why you decided to pursue medical school in the first place, to seek a
higher level of knowledge. The diagnostic pathways assumed during your previous career
were geared towards a certain threshold, and thinking beyond this into continuity of care
is now your prime motive. For example, as a paramedic we are taught to stabilize a
patient to the best of our ability; however, we have minimal concern about the
longitudinal outcome of the patient. As an aspiring physician, you are also thinking in the
here and now, but also the long-term effects that can result directly from your actions. - Utilizing your skills in a previous profession to better yourself as a medical student.
What many former practitioners don’t realize as medical students is that they are still an
integral part of the team, where they can use their experience of the past to assist in ways
those without prior applicable skills cannot. However, you must understand that your
actions are not under your licence, but under the licence of the resident, fellow and/or
attending. Just because you may have placed chest tubes and central lines in the past
doesn’t mean you will during clinical rotations based on the previous fact. Showing your
confidence and familiarity with certain skills will inspire preceptors to allow you to go
beyond the medical students “scope of practice”, but this should not be expected. Utilize
your abilities to assist your team wherever they may need it, and this might mean cleaning
up the stool once in a while regardless of your practical history. - How to defuse after being pushed to the sidelines during patient care when you
know what needs to be done next. The most notable issue facing those with past
experience is knowing what needs to be done next, but your input being essentially
thwarted. The best example of this for paramedics will be during resuscitations. It is
difficult to watch a tube being misplaced, or an IV being done when an IO is indicated,
but the primary purpose of your transition to medical school was to understand the next
steps (thinking beyond just the resuscitation). Defusing after these situations is important,
as frustrations can build if you continue to concern yourself with these circumstances.
Talk with a resident you are comfortable with, as they may have similar feelings. Chat
with an old co-worker who you can comfortably convey your thoughts to. They may be
able to offer further insight, especially into affairs you may not have considered, such as:
“What is the definitive care for this patient?” Maybe it’s ECMO for that massive PE, or
bronchoscopy for an FBO that can’t be visualized. These are all steps you may be less
familiar with, and are being thought of at the time by the primary team, rather than the
basics such as IVs and intubation.
As previous healthcare practitioners you have transitioned to a very difficult time in your life,
becoming a student once again. With this, issues will arise that are not common to the average
medical student who goes directly from undergraduate studies to medical school. However,
remembering why you decided to become a physician in the first place is key. Not only can you
bring a distinct level of understanding to your clinical studies, but your prior experience can be
beneficial to the primary team while you simultaneously strengthen your knowledge in becoming
a future physician.
Related Content

Jun 11, 2021
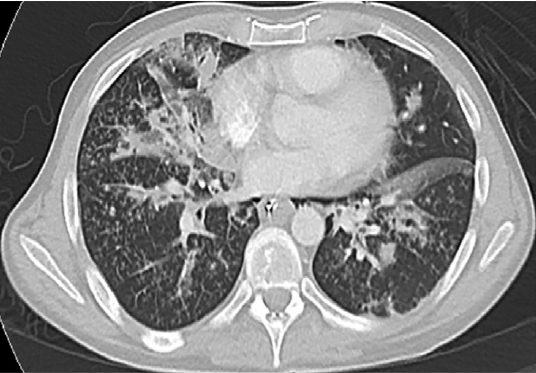
Pulmonary Manifestations Following IV Injection of Crushed Suboxone: A Case of Excipient Lung Disease
Include excipient lung disease (ELD) in the differential diagnosis when evaluating and treating a patient with a history of intravenous drug use presenting with respiratory failure and typical findings on chest imaging.




