Metformin-associated lactic acidosis (MALA) is an unusual complication in the setting of metformin use or overdose. This condition is often a diagnosis of exclusion due to its rarity compared with more common causes of anion gap metabolic acidosis such as septic shock, diabetic or alcoholic ketoacidosis, toxic ingestion, and renal failure.
MALA has a 30-50% risk of mortality, especially in patients presenting with pH <7.1 or lactic acid >25 mmol/L.1-3 Aggressive supportive care is necessary to improve survivability.
We present a suspected case of MALA requiring intensive, collaborative medical care among emergency medicine, critical care, nephrology, toxicology, and internal medicine allowing for a remarkable patient recovery.
Case Presentation
A 58-year-old man with a history of hypertension, type 2 diabetes mellitus, remote alcohol use disorder, and suicide attempt (nearly 30 years ago) arrived at the ED via EMS for altered mental status and frequent falls within the previous 24 hours. The patient’s roommate called medics and provided history at the scene. For EMS, the patient initially moved all extremities and was mildly combative and then became somnolent during transport. ED personnel did not record initial EMS vital signs.
Upon arrival at the ED, the patient had a Glasgow Coma Scale (GCS) of 3, indicating a high risk of impending brain injury or death. His initial vital signs included heart rate of 112 beats per minute, blood pressure of 94/50 mmHg, respiratory rate of 28 breaths per minute, rectal temperature of 90.4 degrees Fahrenheit, and pulse oximetry of 86% on 15 liters/minute of oxygen using a non-rebreather mask.
The patient’s ECG revealed atrial fibrillation with a ventricular rate of 108, incomplete left bundle branch block, and nonspecific ST segment abnormalities concerning for possible lateral subendocardial injury. These ECG findings heightened consideration of acute coronary syndrome, cardiomyopathy, or massive pulmonary embolism.
Oral intubation was performed for both airway protection and emergent management of acute hypoxic respiratory failure. An initial 1 liter IV fluid bolus of sodium chloride 0.9% solution was administered to enhance the patient’s mean arterial pressure. Additionally, an external convection warming unit (3M™ Bair Hugger™) was applied to manage the patient’s hypothermia.
Given the abnormal vital signs, sepsis of unknown origin was likely for this patient. Consequently, broad-spectrum antibiotics consisting of vancomycin and a blend of piperacillin and tazobactam were administered. Additionally, the patient received 30 milliliters/kilogram of IV isotonic crystalloid fluids in compliance with current sepsis guidelines. Despite fluid resuscitation, the patient remained hypotensive, prompting the initiation of 2 IV vasopressors, norepinephrine bitartrate and vasopressin.
Upon electronic chart review, the patient’s home medications included metformin, insulin, oxycodone, and aspirin. Earlier in the day, the patient had contacted his primary care provider’s office complaining of fatigue, generalized malaise, and shortness of breath, and he was referred to the ED.
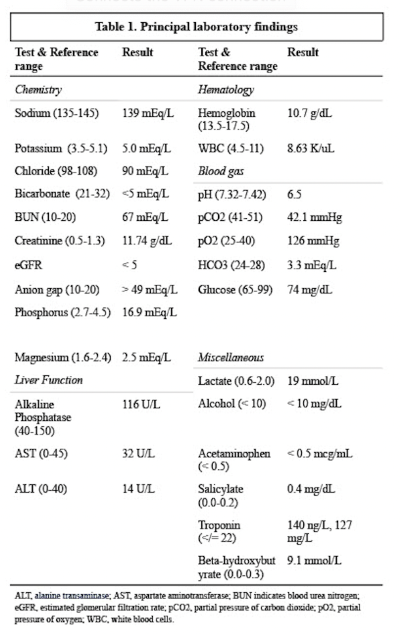
Noteworthy initial lab results included a venous blood gas (VBG) revealing pH of 6.5, bicarbonate of 3.3 mEq/L, and partial pressure of carbon dioxide (pCO2) 42.1 mm/Hg, consistent with a combined metabolic and respiratory acidosis with a superimposed metabolic alkalosis. His anion gap was greater than 49 mEq/L.
Given the patient’s profound anion gap metabolic acidosis and lactic acidosis, further investigation for possible toxic ingestants, such as alcohol, ethylene glycol, methanol, salicylates, and acetaminophen, were pursued.
Additional lab testing revealed blood urea nitrogen (BUN) of 67 mEq/L, creatinine of 11.74 g/dL, and glomerular filtration rate (GFR) of 5, indicative of acute renal failure. (Approximately 5 months prior to presentation, the patient’s baseline creatinine was 1.2 g/dL.) His beta-hydroxybutyrate was significantly elevated at 9.1 mmol/L, presuming a marked ketotic state, but blood glucose was within normal range, making diabetic ketoacidosis or hyperosmotic hyperglycemic syndrome a less likely etiology for his metabolic derangement. Remaining ED lab studies included unremarkable liver function testing and CBC. Salicylate, acetaminophen, and ethanol blood levels were negative for elevation.
Advanced radiological imaging was performed due to the patient’s altered mental status and recent history of falls. This imaging included CTA head and neck, CT pulmonary arteries, CT abdomen and pelvis with IV contrast, and CT cervical, thoracic, and lumbar spine without contrast. All imaging studies were negative for acute pathology or evidence of recent traumatic injuries.
The emergency physician initiated a sodium bicarbonate IV infusion to address the patient’s profound acidotic state. Nephrology agreed with the continuation of this treatment and recommended initiating emergent dialysis with continuous renal replacement therapy (CRRT) after the patient’s arrival to the ICU. This constant, 24-hour-per-day dialysis treatment allows for steady correction of ongoing acidosis and electrolyte derangements in hemodynamically unstable individuals with acute renal failure. CRRT can also improve uremia and assist with clearance of dialyzable toxins.
On the patient’s arrival to ICU, the intensivist contacted the poison control center due to concerns for possible toxic ingestion. The center’s toxicologist advised starting both IV fomepizole and high-dose vitamin therapy due to the potential of ethylene glycol or methanol toxicity as a contributor to the patient’s anion gap metabolic acidosis and renal failure. Both therapies were initiated, and the toxicologist remained in communication with the critical care team in the days following.
During the initial ICU course, the patient’s condition continued to decline, requiring the addition of epinephrine for vasopressor support and stress dose steroids. Despite these additional supportive therapies, the patient’s acidosis continued to deteriorate. His pH became undetectable on blood gas machine analysis, indicating a level lower than the machine’s cut-off value of 6.5. IV sodium bicarbonate ampules were administered in addition to the sodium bicarbonate infusion to correct the ongoing metabolic derangements.
Despite significant resuscitative measures, including 3 vasopressors, sodium bicarbonate infusion and boluses, and CRRT, the patient’s metabolic acidosis and hemodynamic instability continued to worsen. His prognosis remained poor, and he was now considered in refractory shock. Due to this, methylene blue was administered as an IV bolus followed by tapper. The hope was that it would act as a vasopressor-sparing agent in vasoplegic, distributive shock. It acts to inhibit nitric oxide synthesis, thereby alleviating vasoplegia and promoting an increase in blood pressure.4,5
On hospital day 2, marked improvement occurred in the patient’s clinical status after initiating methylene blue. Due to progressive resolution in the patient’s metabolic state, the intensivist discontinued the sodium bicarbonate infusion. Additionally, as the patient demonstrated consistent improvement in his mean arterial pressure, 2 of the vasopressors at maximum dose were steadily weaned and then discontinued, leaving only norepinephrine bitartrate.
The patient continued to make significant clinical improvements. On hospital day 3, now off vasopressors, his CRRT was transitioned to intermittent hemodialysis (HD). Following negative blood culture results, antibiotics were discontinued on the 5th day of hospitalization, and the patient underwent a successful extubation. After a steady improvement in alertness, the intensivist questioned the patient about the circumstances leading to his medical emergency, but unfortunately, he did not recall any imperative details. He denied any intentional ingestions or suicidal ideation leading up to his hospitalization. His expanded drug screen and volatile panel only demonstrated an elevated acetone level of 11, likely due to his initial severe ketotic state.
Renal recovery and urine production returned for the patient during his hospitalization, so intermittent HD ceased after 3 sessions on hospital day 9. The following day, he was transferred to a regular medical floor with a relatively uneventful recovery, except for episodes of delirium. After 3 weeks of hospitalization, the patient was discharged home with weekly outpatient physical therapy sessions.
Given the lack of any other identified etiology for the patient’s profound metabolic acidosis, the multidisciplinary care team surmised that the patient experienced MALA in the setting of metformin use. Most likely, an unspecified illness led to dehydration and AKI, which contributed to the development of this rare disorder in the days preceding his hospitalization.
Discussion
Metformin is a biguanide anti-hyperglycemic agent commonly prescribed for patients with type 2 diabetes mellitus and polycystic ovary syndrome. This oral medication is not metabolized by the liver and is excreted unchanged in the urine.1 Due to its unique pharmacokinetics, metformin can accumulate in the body during times of acute kidney injury or in patients with a history of chronic kidney disease.1-3 As a biguanide, metformin has a well-established risk of lactic acidosis, though much lower than phenformin, an antihyperglycemic medication of the same class.1
Metformin’s mechanism of action causes increased lactate production by blunting hepatic gluconeogenesis.3 This disruption in metabolism leads to increased pyruvate production, resulting in elevated lactic acid, and thus increased serum lactate levels.1-3
Metformin-associated lactic acidosis is defined as an elevated lactic acid and metabolic acidosis in the setting of metformin use with numeric values of pH <7.35 and lactate >5 mmol/L.1

Due to this drug’s action on the liver, MALA starts as a type B lactic acidosis as it alters pyruvate metabolism in the Cori cycle at the mitochondrial level. This type of acidosis occurs from impaired cellular functioning, while type A lactic acidosis is defined by tissue hypoxia and impaired tissue perfusion.5
Even though MALA starts as type B lactic acidosis, it can progress to include type A because of compounding, multifactorial organ dysfunction leading to hemodynamic instability, tissue hypoperfusion, and hypoxia.6,7 MALA can provoke vasoplegic shock, with a profoundly low systemic vascular resistance. Vasoplegic shock is a type of distributive shock with smooth muscle derangement causing abnormal vasoconstriction leading to systemic hypoperfusion.
A test obtaining serum level of metformin is not readily available and offers little utility in making the diagnosis or predicting the severity of MALA.3 As a result, such testing is infrequently ordered.8 Mortality is more readily predicted in MALA by a pH <6.9 and serum lactate >25 mmol/L.3,9
One retrospective study in the ED suggested that MALA should be suspected in patients with septic shock who take metformin and have a serum lactate >8.4 mmol/L and creatinine >2.9 mg/dl.3,6 When these criteria were met, the specificity of MALA was 99 percent.3,9
Management
Management of this disorder is primarily supportive with the goal of correcting underlying lab derangements created by vasoplegic shock. Sodium bicarbonate infusions are suggested in pH <7.15.10 Hemodialysis is recommended if the patient demonstrates severe metabolic acidosis pH <7.1 and lactic acid concentration >20 mmol/L. HD can also be indicated if the patient’s acid-base disorder fails to improve in 2-4 hours of bicarbonate therapy or if there is presence of shock, kidney injury, or liver injury.3
Methylene blue has been used for refractory shock, but its utility and wide acceptance is limited due to a lack of controlled studies. Although its mechanism of action is unclear, it is thought to inhibit nitric oxide production, thereby helping to restore vascular tone.11-13 Additionally, it has a catecolamine-sparing effect through its action against guanylyl cyclase for patients with distributive shock.4,5
While methylene blue has been well-established in vasoplegic shock in cardiothoracic surgery patients, its utility as an adjunct to vasopressors is not as frequently employed.13 There are a few other case reports of methylene blue use in MALA patients who showed significant improvement in vasoplegic shock when it was used as an adjunct to routine vasopressors.11,12
Conclusion
MALA is a difficult diagnosis to make due to lack of specific lab testing revealing toxicity. However, this disorder should be considered in patients presenting with marked hemodynamic instability with strikingly elevated lactic acid levels, whose home medication list includes metformin.
The incidence of MALA may increase, given the rising prevalence of type 2 diabetes mellitus and the preference for metformin as the disease’s initial treatment of choice.
Notwithstanding, effective interdisciplinary care, with a focus on supportive care measures, can result in the best possible outcome for MALA patients. Adjunctive therapies are likely to be necessary in MALA, and the use of methylene blue has shown anecdotal benefit in some case reports. Further investigation is necessary to enhance our understanding of the utility of using methylene blue in refractory hemodynamic instability in non-traumatic medical emergencies.
References
- Dyatlova N, Tobarran NV, Kannan L, et al. (2023) Metformin-Associated Lactic Acidosis (MALA). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. https://www.ncbi.nlm.nih.gov/books/NBK580485/.
- Van Berlo-van de Laar IRF, Gedik A, van 't Riet E, de Meijer A, Taxis K, Jansman FGA. Identifying patients with metformin associated lactic acidosis in the emergency department. Int J Clin Pharm. 2020 Oct;42(5):1286-1292. doi: 10.1007/s11096-020-01069-2. Epub 2020 Sep 22. PMID: 32960426; PMCID: PMC7522070.
- Chu, J., Stolbach, A., Hendrickson, R. & Ganetsky, M. (2022) Metformin poisoning. Up-to-Date. Last updated August, 2022. https://www.uptodate.com/contents/metformin-poisoning.
- Puntillo F, Giglio M, Pasqualucci A, Brienza N, Paladini A, Varrassi G. Vasopressor-Sparing Action of Methylene Blue in Severe Sepsis and Shock: A Narrative Review. Adv Ther. 2020 Sep;37(9):3692-3706. doi: 10.1007/s12325-020-01422-x. Epub 2020 Jul 23. PMID: 32705530; PMCID: PMC7444404.
- Naoum, E.E., Dalia, A.A., Roberts, R.J. et al. Methylene blue for vasodilatory shock in the intensive care unit: a retrospective, observational study. BMC Anesthesiol 22, 199 (2022). https://doi.org/10.1186/s12871-022-01739-w.
- Foucher CD, Tubben RE. Lactic Acidosis. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470202/.
- Lazarus, B., Wu, A., Shin, J. I., Sang, Y., Alexander, G. C., Secora, A., Inker, L. A., Coresh, J., Chang, A. R., & Grams, M. E. (2018). Association of Metformin Use With Risk of Lactic Acidosis Across the Range of Kidney Function: A Community-Based Cohort Study. JAMA internal medicine, 178(7), 903–910. https://doi.org/10.1001/jamainternmed.2018.0292.
- Dell'Aglio DM, Perino LJ, Kazzi Z, Abramson J, Schwartz MD, Morgan BW. Acute metformin overdose: examining serum pH, lactate level, and metformin concentrations in survivors versus nonsurvivors: a systematic review of the literature. Ann Emerg Med. 2009 Dec;54(6):818-23. doi: 10.1016/j.annemergmed.2009.04.023. Epub 2009 Jun 25. PMID: 19556031.
- Blumenberg, A., Benabbas, R., Sinert, R., Jeng, A., & Wiener, S. W. (2020). Do Patients Die with or from Metformin-Associated Lactic Acidosis (MALA)? Systematic Review and Meta-analysis of pH and Lactate as Predictors of Mortality in MALA. Journal of medical toxicology : official journal of the American College of Medical Toxicology, 16(2), 222–229. https://doi.org/10.1007/s13181-019-00755-6.
- Blough, B., Moreland, A., & Mora, A., Jr (2015). Metformin-induced lactic acidosis with emphasis on the anion gap. Proceedings (Baylor University. Medical Center), 28(1), 31–33. https://doi.org/10.1080/08998280.2015.11929178.
- Graham RE, Cartner M, Winearls J. A severe case of vasoplegic shock following metformin overdose successfully treated with methylene blue as a last line therapy. BMJ Case Rep. 2015 Jul 6;2015:bcr2015210229. doi: 10.1136/bcr-2015-210229. PMID: 26150642; PMCID: PMC4493209.
- Plumb B, Parker A, Wong P. Feeling blue with metformin-associated lactic acidosis. BMJ Case Rep. 2013 Mar 1;2013:bcr2013008855. doi: 10.1136/bcr-2013-008855. PMID: 23456165; PMCID: PMC3618850.
- Sari-Yavuz, S., Heck-Swain, K. L., Keller, M., Magunia, H., Feng, Y. S., Haeberle, H. A., Wied, P., Schlensak, C., Rosenberger, P., & Koeppen, M. (2022). Methylene blue dosing strategies in critically ill adults with shock-A retrospective cohort study. Frontiers in medicine, 9, 1014276. https://doi.org/10.3389/fmed.2022.1014276.



