Case Presentation
A 15-year-old male arrives via EMS approximately 1 hour after an intentional overdose of an estimated 20-25 0.3 mg tablets of clonidine. The patient denied co-ingestion with other agents. Triage blood pressure was 107/74 with heart rate of 84 bpm. The patient was initially drowsy but awake and oriented. However, the patient became more somnolent throughout the ED course, approximately 80 minutes post-ingestion. He became bradycardic and hypotensive and was minimally responsive with markedly reduced respirations.
Discussion
Clonidine was initially marketed as a nasal decongestant. However, a commonly observed side effect was hypotension, leading toward its use as an antihypertensive agent.1 Although clonidine is primarily used for hypertension, it can also be a useful treatment for other conditions including ADHD, Tourette’s syndrome, cancer-related pain, neonatal opioid withdrawal syndrome, alcohol or opioid withdrawal, anxiety, PTSD, restless leg syndrome, menopausal hot flashes, and vascular migraine prophylaxis. It can be administered via oral tablets, oral suspension, injectable solution, transdermal patch, and topical cream.2
Clonidine acts on a2-adrenergic receptors in the CNS, which inhibits the release of peripheral catecholamines. This leads to a decrease in heart rate, cardiac contractility, and peripheral vascular resistance. The sympatholytic effect is modulated by nitric oxide and gamma-aminobutyric acid, which can lead to variability on the individual level in presentation of toxicity.3,4,5
Additionally, clonidine has been shown to activate I1-imidazoline receptors, which also has an antihypertensive effect.6
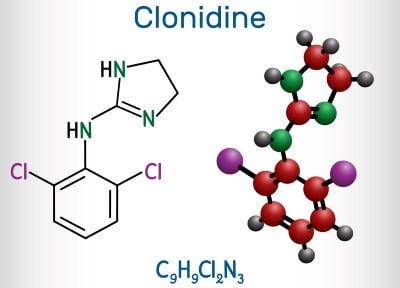
It has been proposed that clonidine may promote the release of endogenous opioids and/or directly stimulate opioid receptors.7,8 The opioid-like effect is believed to be from interaction with I2-imidazoline receptors, which are involved in pain reception modulation, as well as promotion of β-endorphin release, which can directly interact with opioid receptors.9
Because of its mechanism of action, clonidine toxicity may present as bradycardia, hypotension, decreased respiratory rate, and CNS depression. In some cases, patients may present with hypertension, especially shortly after ingestion or exposure.10
The onset of action is typically 30-60 minutes after ingestion.11 Clonidine reaches peak serum around 2-3 hours, and effects can last up to 8 hours.12 It is found to be 20-40% bound to protein in circulation. The majority is renally excreted.13 The pharmacokinetics may vary based on a patient’s serum protein concentration, metabolic rate, and renal function.
Overdoses can be intentional or accidental. In intentional overdose, clonidine is often co-ingested with other agents. Compounding abnormalities can lead to accidental overdose, as it can be unclear how large of a dose is being administered.14 Although overdose is typically seen with oral formulations, there has been documentation of overdoses with topical formulations, especially within the pediatric population.15,16
Effects of overdose can vary based on the dose ingested and the patient’s age. Adult patients may be asymptomatic or have mild effects, while a single tablet can lead to significant symptoms in a child.17 Differences between different age groups within pediatric patients have been observed, as younger children present with severe bradycardia while severe hypotension is seen more in adolescents.18
Management
Management of clonidine overdose is case-dependent. Clonidine is not included in most serum or urine assays. The diagnosis of acute toxicity is based on historical information or clinical suspicion based on patient presentation and hemodynamic abnormalities.
The mainstay of treatment is supportive care. Evaluation of airway compromise, breathing abnormalities, and cardiovascular disruption should take precedence. Endotracheal intubation may be considered but comes with the risk of increased morbidity and longer hospital stay. Supplemental oxygen also may be considered. Hypotension may be addressed with crystalloid fluid resuscitation. Symptomatic bradycardia may be treated with atropine. In severe and prolonged hypertension, antihypertensive agents such as nicardipine or nitroprusside can be used. Historically, tolazoline, furosemide, and diazoxide have also been used successfully.19.20.21
Naloxone administration has been shown to have a beneficial effect in acute clonidine toxicity, especially in pediatric patients with CNS depression. This is likely due to the association of endogenous opioid release and agonism of opioid receptors. Dosage of naloxone for reversal may be higher than exogenous opioid reversal and can be up to 10 mg. Repeat administration may be necessary. In rare instances, naloxone infusions have been utilized after boluses. Naloxone administration usually improves somnolence, but patients may remain persistently bradycardic. Patients may also experience transient hypertension after administration, but this typically self-resolves.22
Naloxone may not be beneficial in some cases. In a study focused on adult patients, naloxone administration was not clinically significant.23 Some pediatric cases are refractory to naloxone but responsive to isotonic crystalloid and atropine.24
However, naloxone has a safe drug profile and has not been shown to produce adverse effects when used for clonidine toxicity reversal. It can reduce the need for endotracheal intubation and CT imaging in pediatric patients, thus decreasing morbidity and mortality. Therefore, it should be considered.22
Case Resolution
EKG showed sinus bradycardia with incomplete right bundle branch block. Laboratory studies — including CBC with differential, CMP, serum toxicology, and urine drug screen — were within normal limits. Given the decline in mental status and worsening vital signs, the patient was given a 4 mg IV bolus dose of naloxone, with no improvement. After an additional 6 mg bolus dose of naloxone, the patient immediately became more alert. He was subsequently placed on a naloxone infusion at 10 mg/hr and admitted to the pediatric ICU. The patient did not require additional medical intervention and was discharged to an inpatient psychiatric facility after a 2-day ICU course.
Conclusion
Clonidine is a widely available drug and has been seen as the culprit in an increased number of intentional and accidental overdoses. Symptoms of toxicity include hypertension or hypotension, bradycardia, respiratory depression, and CNS depression. The mainstay of treatment is supportive care. Naloxone may play a role in pediatric patients with CNS depression and can decrease the need for endotracheal intubation and improve morbidity. Clinicians should be cognizant that higher than typical doses for opioid overdose may be required when clonidine ingestion is suspected or known.
References
- Higgins GL, Campbell B, Wallace K, TalbotS. Pediatric poisoning from over-the-counter imidazoline-containing products. Ann Emerg Med. 1991;20(6):655-658.
- Yasaei R, Saadabadi A. Clonidine. StatPearls. 2023. Accessed December 4, 2023. https://www.ncbi.nlm.nih.gov/books/NBK459124/.
- Castro JL, Ricci D, Taira CA, Ramirez A. Central benzodiazepine involvement in clonidine cardiovascular actions. Can J Physiol Pharmacol. 1999;77(11):844-851.
- Gozlinska B, Czyzewska-Szafran H. Clonidine action in spontaneously hypertensive rats(SHR) depends on the GABAergic system function. Amino Acids.1999;17(2):131-138.
- Venturini G, Colasanti M, Persichini T, Fioravanti E, Federico R, Ascenzi P. Selective inhibition of nitric oxide synthase type I byclonidine, an anti-hypertensive drug. Biochem Pharmacol.2000;60(4):539-544.
- Ernsberger P, Friedman JE, Koletsky RJ. The I1-imidazoline receptor: from binding site to therapeutic target in cardiovascular disease. J Hypertens Suppl. 1997;15(1):S9-23.
- Swift A, Wilson M. Reversal of the effects of clonidine using naloxone. Anaesth Rep. 2019;7(1):4-6.
- Mastrianni JA, Abbott FV, Kunos G. Activation of central mu-opioid receptors is involved in clonidine analgesia in rats. Brain Res. 1989 Feb 13;479(2):283-9.
- Zheng X, Zhang T, Ding H, Wang C. Plasma levels of beta-endorphin, leucine enkephalin and arginine vasopressin in patients with essential hypertension and the effects of clonidine. Int J Cardiol. 1995;51(3):233-244.
- Spiller HA, Hays HL, Aleguas A Jr. Overdose of drugs for attention-deficit hyperactivity disorder: clinical presentation, mechanisms of toxicity, and management. CNS Drugs. 2013;27(7):531-43.
- Dollery CT, Davies DS, Draffan GH, Dargie HJ, Dean CR, Reid JL, Clare RA, Murray S. Clinical pharmacology and pharmacokinetics of clonidine. Clin Pharmacol Ther. 1976;19(1):11-17.
- Lin MT, Chandra A, Ko WC, Chen YM. Serotonergic mechanisms of clonidine-induced hypothermia in rats. Neuropharmacology. 1981;20(!):15-21.
- Lowenthal DT. Pharmacokinetics of clonidine. J Cardiovasc Pharmacol. 1980;2(suppl 1):S29-37.
- Barbuto AF, Burns MM. Clonidine compounding error: bradycardia and sedation in a pediatric patient. JEM. 2020; 59(1):53-55.
- Cates AL, Wheatley SM, Katz KD. Clonidine Overdose in a Toddler Due to Accidental Ingestion of a Compounding Cream. Pediatr Emerg Care. 2018;34(4):e79-e81.
- Horowitz R, Mazor SS, Aks SE, Leikin JB. Accidental clonidine patch ingestion in a child. Am J Ther. 2005;12(3):272-4.
- Spiller HA, Klein-Schwartz W, Colvin JM, Villalobos D, Johnson PB, Anderson DL. Toxic clonidine ingestion in children. J Pediatr. 2005;146(2):263-6.
- Duong C, Lovett C, Downes MA, Isbister GK. Reality of clonidine poisoning in children and adolescents. J Paediatr Child Health. 2023;59(6):827-832.
- Schieber RA, Kaufman ND. Use of tolazoline in massive clonidine poisoning. Am J Dis Child. 1981;135(1):77-8.
- Marruecos MD, Rogland A, Frati ME, Artigas A. Clonidine Overdose. Crit Care Med. 1983;11(12):959-960.
- Hunyor SN, Bradstock K, Somerville PJ, Lucas N. Clonidine overdose. Br Med J. 1975;4(5987):23.
- Seger DL, Loden JK. Naloxone reversal of clonidine toxicity: dose, dose, dose. Clin Toxicol (Phila). 2018 Oct;56(10):873-879.
- Isbister GK, Heppell SP, Page CB, Ryan NM. Adult clonidine overdose: prolonged bradycardia and central nervous system depression, but not severe toxicity. Clin Toxicol (Phila). 2017;55(3):187-192.
- Ahmad SA, Scolnik D, Snehal V, Glatstein M. Use of naloxone for clonidine intoxication in the pediatric age group: case report and review of the literature. Am J Ther. 2015;22(1):e14-6.



