Medical Transition
Many transgender men and women take hormonal medications to help align their body with their identities. For trans women this mostly consists of estrogen and anti-androgens. These medications lead to many changes in the body such as stopping facial hair growth, body fat redistribution, breast development, and even lactation in some cases. In trans men, this is usually just testosterone, which conversely leads to body and facial hair growth, increased muscle mass, fat redistribution into more male patterns, and clitoral enlargement. While many trans individuals welcome these changes, different people have different ideas about how masculine or feminine their bodies should look, so they may take different amounts of hormones to best align their bodies with how they feel. Some effects of these medications can be more stressful for patients; for instance estrogen can lead to decreased erectile function, while testosterone can lead to hair loss. In addition, these medications typically require a prescription, and depending on state regulations, patients may need a written letter from a mental health professional to begin hormone therapy.
While medical transition is often more attainable for patients than surgery because of cost, it can still be difficult to get access to licensed providers, and some of your patients may get hormones from black market providers, online, or internationally. Some may even use other non-traditional chemicals to alter their hormones in other ways. The most important things to remember are that hormonal changes happen gradually over months to years, some are reversible in varying degrees, and different patients may feel positively or negatively about the resulting changes to their body.
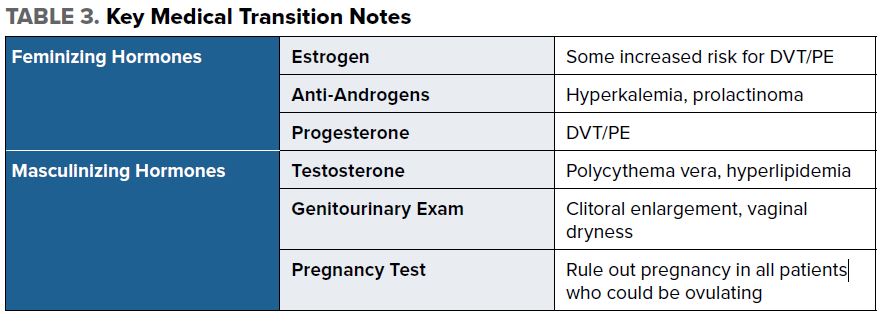
Feminizing Hormones
Estrogen
Estrogen is the most common feminizing medication that your female identifying trans patients may be taking. As with cisgender women, venous thromboembolus (VTE) is one of the more common complications of exogenous estrogen use.6 Again, as in cisgendered women, this risk is further increased in smokers, patients over the age of 40, those with prolonged immobilization or sedentary lifestyles, the obese, and those with underlying thrombophilic disorders.6 Most women use injectable steroids, although some may prefer pills, patches, or creams. The rate of VTE is decreased with transdermal estrogen.6 However, many trans women report that feminizing effects happen more slowly with transdermal estrogen, so it is not as popular. There is data to support the idea that estrogen may increase the risk of cardiovascular disease in patients over 50 with underlying risk factors.7
Anti-androgens
Most trans women take anti-androgens in addition to estrogen. These drugs reduce endogenous testosterone levels and activity, which then decreases the dose of estrogen needed to suppress the effects of testosterone on the feminizing body, as well as help with a more feminine body fat distribution.8 The most common of these is spironolactone, which can cause diuresis and hyperkalemia, as well as the development of high prolactin levels and even prolactinoma.9 Many trans women also take finasteride or dutasteride, 5-alpha reductase inhibitors that decrease the peripheral conversion of testosterone to DHT, which is the hormone that often contributes to body hair and male pattern baldness.8
Progesterone
Progesterone is a controversial medication in the transfeminine community. Some trans women report that it increases energy, libido, and improves breast development and body fat redistribution.10 However, there is very little data to support those claims. In addition, progesterone may further increase the risk of blood clots.
Masculinizing Hormones
Most trans men only take testosterone, as no medication is needed to suppress estrogen production in order to see masculinizing effects. This is usually taken as an injectable intramuscular shot, although some trans men prefer to use patches or creams.8 Although there is limited data, some anecdotal evidence does suggest that masculinizing effects take longer with transdermal testosterone.8 There are limited side effects of testosterone, but there is an increased risk of polycythemia vera, as well as increased LDL and triglyceride levels. Most trans men on testosterone will not ovulate and therefore not have a menstrual cycle, making pregnancy impossible. However, if dosing has been irregular or lower than necessary to suppress this cycle, ovulation and pregnancy are possible. Thus, it is important to rule out pregnancy in all of your patients with ovaries.