EMRA’s Detailed Responses to the ACGME Proposed Changes to Emergency Medicine Training
The EMRA Board of Directors studied the full proposal set forth by the ACGME Review Committee for Emergency Medicine. (Please see our review of the most concerning proposed changes here.)
Following are EMRA’s detailed responses, based on the EMRA Representative Council’s existing policies and member feedback.
To fight the proposed changes, we need our emergency medicine community to take action and submit public comments–specifically comments that offer alternative solutions to the current proposals. There is power in numbers, and we need your voice! Please submit comments as an individual as well. It only takes a few simple steps:
- Navigate to the ACGME public comment page
- Fill out the basic information portion (Some fields optional)
- Under the “Requirements for Comment,” select the requirement number (Bolded below)
- Copy and paste EMRA’s recommended comment below (Blue text and text underneath is EMRA's stance and comments) or write your own!
- Note: Comments are restricted to 1600 characters on the ACGME Feedback Form.
Please feel free to copy and paste these comments as you tailor your own feedback to the ACGME. All public comments are due May 1.
*Requirements with EMRA's recommended comments
Find EMRA's comments quickly:
Requirement 1.6.b
The addition of participating sites routinely providing any required experience, regardless of length, must be submitted through ADS, and if the participating site is more than 60 miles away, it must be approved by the Review Committee prior to the residents starting the experience. (Core)
EMRA supports this change, with caution.
EMRA supports the spirit of this change but encourages programs to offset the burden on trainees by providing funding to defray the costs associated with compliance.
Return to TopRequirement 1.6.f
Programs must utilize at least one high-resource emergency department and at least one low-resource emergency department for training in emergency medicine. (Core)
EMRA questions this change.
EMRA supports the intent but is unsure the current requirement will meet that intent.
Per EMRA policy, “EMRA recommends Emergency Medicine residency programs partner with Rural and/or Critical Access Hospitals in order to offer or incorporate rotations for residents at these centers as able. EMRA encourages residency programs to explore options to help fund or defray costs residents may incur from participating in rotations at Rural or Critical Access Hospitals.” We believe the intent of this requirement is similar to the intent of this policy, which is to ensure residents are prepared to practice in all environments and have optimal exposure opportunities during training.
We are concerned that “high-resource ED” and “low-resource ED” need to be better defined to ensure residents will gain the desired experience. We encourage ACGME to more clearly define these types of EDs in such a way that ensures the intent of the requirement will be met. This could perhaps be accomplished using metrics such as the percentage of patients transferred or number of available diagnostics/interventions on-site.
Return to TopRequirement 1.8.b.8
Removes the requirement to provide appropriate security services and systems to ensure a safe working environment.
EMRA opposes this change.
The ACGME must support the protection of emergency medicine trainees through its mandates, including the requirement for security services and systems in our EDs. While most EDs do have security forces and plans, workplace violence is a major problem in emergency medicine. Now is not the time to remove this requirement. ACGME needs to publicly continue its support of resident safety by keeping this requirement.
Return to TopRequirement 1.8.h
The aggregate annual volume of patients in the emergency department at the primary and participating emergency department sites must total at least 3,0001 patient visits per approved resident position in the program, determined via a calculation defined by the Review Committee. (Core)
EMRA opposes this change.
While we believe this requirement moves toward residents seeing a certain volume of patients throughout the course of training, we think the intent is overshadowed by several flaws and/or poor assumptions in the proposed calculations. We should work to find a better alternative.
EMRA proposes that residents be required to have a minimum of 5,000 patient encounters throughout their residency.
This approach has multiple benefits. First, it guarantees a number of encounters, which would ensure correction of the trend ACGME has cited of decreased patient encounters. It would also negate any need for the complicated formulas currently proposed. While these formulas exist in hopes of ensuring an adequate number of patients are available to residents, they do not guarantee that residents are seeing those patients. The only way to ensure residents are getting enough patient encounters would be to mandate a minimum number of encounters.
Return to TopRequirement 1.8.j
The aggregate annual volume of critical care patients at the primary and participating emergency department clinical sites must total at least 120 critical care patients per approved resident position in the program, determined via a calculation defined by the Review Committee. (Core)
EMRA opposes this change.
EMRA suggests residents be required to have a minimum of 180 critical care patient encounters in the Emergency Department throughout their training. These should be counted from those admitted to ICUs, step-down units, operative care, interventional or cardiac suites, or the morgue following treatment in the ED.
Similar to 1.8.h, the proposed calculation is complicated and does not adequately estimate the number of critical care patients a resident will manage. Rather than just ensuring availability, we need to ensure residents are seeing the available patients. Similar to our argument in 1.8.h, the only way to ensure residents get the desired number of patient encounters is to mandate a minimum and track it.
180 represents 3% of the 6,000 patient encounters (5,000 adult + 1,000 pediatrics) as outlined in our other recommendations. Additionally, we oppose the carve out that allows for additional ICU rotations if ED critical care volumes are not met. ED management of a critical patient is very different from ICU management of a critical patient, and ICU experience is not a substitute for critical ED patients. We believe this approach better sets expectations for programs and will lead to a better educational experience for residents.
Return to TopRequirement 1.11.a
The Sponsoring Institution and the program must ensure that patient care experiences, including procedures and resources, are distributed across education and training programs in a manner that supports the educational needs of emergency medicine residents. (Core)
EMRA supports this change without comment.
Return to TopRequirement 2.5.d
The program director must have demonstrated experience in an educational leadership role. (Core)
EMRA supports this change.
We agree program directors should have a background as educators in academic medicine and should be familiar with administrative roles within residency/fellowship training.
Return to TopRequirement 2.7.a
There should be faculty members available to the program from within the department or institution with background and focused experience in patient safety, quality improvement, scholarship, ultrasound, and medical education (including simulation) who are actively engaged in the development, implementation, and assessment of their specific areas of curricular content. (Detail)
EMRA supports this change with clarification.
We agree that educators should possess specialized skills, qualifications, and experience in the subject matters they oversee.
Relative to ultrasound faculty, we find this language too vague and open to interpretation. We strongly recommend an explicit requirement for faculty members to be board-certified in Emergency Medicine and possess either an advanced ultrasound fellowship or a Focused Practice Designation in Advanced Emergency Ultrasonography from the American Board of Emergency Medicine. Since ultrasound training varies across institutions, these qualifications would ensure a standardized baseline of expertise, allowing residents to learn through structured, high-quality experiences. Furthermore, advancing residents’ ultrasound education demands high-quality feedback from highly trained educators.
Return to TopRequirement 2.10.e
When faculty members who possess certification other than ABEM or AOBEM supervise residents assigned to a low-resource emergency department or low acuity emergency medicine rotation, this time does not count toward the required 124 weeks of core emergency medicine experience which must occur under the supervision of board-certified emergency medicine physicians. (Core)
EMRA supports this change.
EMRA believes the gold standard for emergency care is that which is provided by board-certified/board-eligible emergency physicians. However, many emergency departments, particularly those in rural and low-resource areas, are staffed by physicians who are not certified by ABEM or AOBEM. A study published in 2021 in the Journal of the American Board of Family Medicine shows that family physicians comprise nearly 10% of the workforce covering emergency departments.
As we work to increase the number of BC/BE emergency physicians who practice in rural and critical access hospitals, we must limit the number of obstacles in their way.
We strongly oppose invalidating the hours worked by residents in rural and critical access hospitals while under physicians boarded in other specialties. Not only does this diminish the value other board-certified physicians are currently bringing to emergency care in our country, but it is also punitive toward the very programs and trainees who are trying to fill the gaps in the EM workforce.
Return to TopRequirement 4.1
The educational program in emergency medicine must be 48 months in duration. (Core)
EMRA opposes this change.
Support EMRA's proposed structure:
- EM: 94 wks & at least 5,000 patient encounters
- Peds: 24 wksPeds EM: 18 wks & 1,000 patient encounters
- ICU: 4 wks (2+ wks in PICU)
- Critical Care: 16 wks (incl. 4 peds)
- OB: 2 wks
- Vacation: 12 wks
- Structured experiences, electives, etc: 12 wks
- We suggest Admin/QA, Tox/Addiction Med, and EMS be structured experiences.
- Downtrending ABEM board pass ratesACGME has offered no evidence to suggest 4-yr graduates are better prepared
- 2023 ABEM study showed 3-yr graduates actually have higher board pass rates
- Thus, citing the downtrend in board pass rates to lengthen training is incongruent with the available evidence
- Decreasing work hours/patient encounters
- RC suggested 124 wks of EM so that an average resident at an average program would have approximately 5,000 adult ED patient encounters
- Time on a rotation only guarantees time on a rotation. Mandating time spent in ED will not guarantee the desired outcome.
- Focusing on minimum # of patient encounters and time in ED will better guarantee the desired outcome while allowing programs more flexibility in curriculum development
- Assuming a mean of 45 hrs/wk in ED, resident would need to average 1.2 patients/hr to meet EMRA's proposed minimum. If programs cannot meet these minimums—whether due to boarding, staffing by APPs, etc.—then they will need to decrease their complements or choose a 4-yr format.
Requirement 4.4
Requirement 4.4.c: Residents must demonstrate competence in selecting, interpreting, and applying appropriate diagnostic and therapeutic modalities based on available resources, including electrocardiography, laboratory, radiography, and point-ofcare ultrasonography based on the probability of disease and the likelihood of test results altering management. (Core)
Requirement 4.4.m: Residents must demonstrate competence in providing care in a variety of practice environments that include critically ill and injured patients, patients with emergent health needs, patients with undifferentiated illness, and lower-acuity patients. (Core)
Requirement 4.4.r: Residents must demonstrate competence in effectively managing and dispositioning patients to facilitate efficient throughput and flow. (Core)
Requirement 4.4.s: Residents must demonstrate competence in reassessing patients and adapting care plans to dynamic changes in patient condition. (Core)
EMRA supports these changes without comment.
Return to TopRequirement 4.5.f
Residents must demonstrate competence in performing common procedures encountered in low-acuity settings. (Core)
EMRA supports this change.
EMRA suggests requiring a minimum number of laceration repairs and I&Ds in the Key Index Procedures. There is agreement that some residents do not get enough experience in these settings and mandating a certain number of these low-acuity procedures is a great method for ensuring accountability to programs and residents.
Return to TopRequirement 4.5.i
Resident procedural experiences must be tracked in the ACGME Case Log System and must meet minimums as defined by the Review Committee. (Core)
EMRA supports this change, with caution.
We agree with the concept of tracking procedure numbers for each EM resident. We also suggest that the number of patient encounters be tracked, which should be done through collaboration with hospital IT departments to minimize burden on residents. We appreciate work has been done to improve the Case Log System and encourage continued efforts to ensure the system is secure, reliable and user-friendly.
Return to TopRequirement 4.5.j.9
Removes "emergency department bedside ultrasound" from the ACGME's list of required procedural competencies.
EMRA opposes this change.
We strongly advocate for ultrasound to remain a key index procedure. POCUS is an essential component of emergency medicine, and is becoming the standard of care in emergency departments across the country. Without adequate training, emergency physicians will inevitably lack confidence in their ability to obtain and interpret ultrasound imaging, and will opt not to use this life-saving diagnostic modality. Developing competency requires structured education, repeated practice, and consistent feedback on image acquisition and interpretation. A minimum scan requirement ensures that all programs dedicate adequate resources to ultrasound training—including equipment, didactic and clinical training time, and feedback platforms such as QPath. Given ultrasound’s pivotal role in rapidly diagnosing critical illness at the bedside and guiding acute management, it should be regarded with the same level of importance as other core resuscitation modalities.
POCUS is cost-effective, noninvasive, and helps avoid radiation. Most importantly, it can be used at the bedside to help expedite diagnosis and guide acute management of critically ill and injured patients, leading to better outcomes for our patients. This success is a direct outcome of the current program requirements, which mandate a minimum number of scans and ensure training from fellowship-trained educators who have the expertise to provide specific structured feedback on technical and interpretative skills.
Return to TopRequirement 4.11.a
Requirement 4.11.a.4: There must be an average of at least five 240 synchronous hours per week of planned didactic experiences annually, exclusive of morning report or change-of-shift teaching developed by the program’s faculty members. (Core)
Requirement 4.11.a.5: REMOVES: Individualized interactive instruction must not exceed 20 percent of the planned didactic experiences. (Core)
Requirement 4.11.a.6: REMOVES: All planned didactic experiences must be supervised by core physician faculty members. (Core)
EMRA supports these changes without comment.
Return to TopRequirement 4.11.a.10
Programs must establish a minimum requirement for conference attendance that meets or exceeds 170 annual hours per resident. (Core)
EMRA supports this change.
We agree with a baseline of 170 annual hours of conference time, on average, during the course of residency. This will allow programs to be flexible with conference attendance throughout the totality of training. For example, some programs have specific years in training that are ICU-heavy, and that often makes conference attendance more difficult, while other years may have rotations during which conference attendance is more easily accomplished. By focusing on the overall average, ACGME would be allowing a healthy degree of flexibility for programs and residents while still ensuring an average of at least 170 hrs/year over the course of residency.
Return to TopRequirement 4.11.b
Experiential Curriculum
The curriculum must include four months of dedicated critical care experiences, including critical care of infants and children. (Core)
EMRA supports this change.
EMRA supports the introduction of Structured Experiences and Rotations and thanks the RC for their innovation in creating this new structure.
EMRA believes that time, in and of itself, guarantees very little in terms of a resident’s educational experience. Additionally, each ED and hospital are different with varying prevalence of different disease processes, competing learners, etc. Thus, we strongly encourage the RC to allow structured experiences for the vast majority of educational experiences and to only mandate a rotation when there is a clearly defined need for the time-based requirement. Structured experiences are much more in line with competency-based medical education compared to time-based rotations.
Return to TopRequirement 4.11.d.1
Emergency Medicine: At least 124 weeks of each resident’s clinical experience must take place in the emergency department under the supervision of emergency medicine faculty members, including. (Core)
EMRA opposes this change.
- Downtrending ABEM board pass rates
- ACGME has offered no evidence to suggest 4-yr graduates are better prepared
- 2023 ABEM study showed 3-yr graduates actually have higher board pass rates
- Another 2023 study did not find any significant differences between 3- and 4-year graduates when comparing metrics related to efficiency, safety and flow in the first year of attending practice
- Thus, citing the downtrend in board pass rates to lengthen training is incongruent with the available evidence
- Decreasing work hours/patient encounters
- RC suggested 124 wks of EM so residents would, on average, have ~5,000 adult ED patient encounters. This end goal can be accomplished in EMRA's proposed 94 weeks.
- Time on a rotation only guarantees time on a rotation. Mandating time spent in ED will not guarantee the desired outcome.
- Focusing on minimum # of patient encounters and time in ED will better guarantee the desired outcome while allowing programs more flexibility in curriculum development
- Assuming a mean of 45 hrs/wk in ED, residents would need to average 1.2 patients per hour to meet EMRA’s proposed minimum. If programs cannot meet these minimums—whether due to boarding, staffing by APPs, etc.—then they will need to decrease their complements or choose a 4-yr format.
Requirement 4.11.d.2.b
At least 62 weeks of the resident’s emergency medicine clinical experience should occur at the primary clinical site. (Detail)
EMRA feels this requirement needs further work.
Some programs have more than 1 "primary site" (eg, consortiums), and others have multiple primary sites that employ the program’s core faculty. There is no data to suggest a single “primary site” leads to better residency education.
Further, EMRA supports a percentage-based approach toward division of training time, rather than a calendar-based approach (eg, 50% of overall ED time should be spent at primary sites, versus 62 weeks of time). We encourage the ACGME to consider the intent behind this requirement and re-engage stakeholders to come up with a requirement that better accomplishes the intent.
Return to TopRequirement 4.11.d.2.c
At least 4 weeks of this clinical experience must be at a low-resource emergency department and 4 weeks at a high-resource emergency department. (Core)
EMRA supports this change, with caution.
We agree with increased experience at low-resource EDs. However, the definition of a “low-resource” ED should be more strictly defined to ensure residents are truly gaining experience that would equip them to practice in the areas where board-certified EM physicians are most needed.
Return to TopRequirement 4.11.d.2.d
At least 4 weeks in the final year must be in a primary patient practitioner role without supervisory responsibilities. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.d.2.f
Residents should have no fewer than 8 weeks of experience in a practice setting designated for low-acuity patients, such as an emergency department fast track or urgent care center. Time spent in a low-resource emergency department does not count toward this experience. (Detail)
EMRA comments on this change.
We agree with the spirit of this proposal, but it needs further clarity. How would this affect programs without a fast track that still see ESI 4 and 5? Rather than basing this requirement on calendar time in a specific type of clinic, we suggest basing it on procedure counts or patient encounters that speak to the heart of the desired competency.
Return to TopRequirement 4.11.d.3
Critical Care: At least 16 weeks of each resident’s clinical experience must be dedicated critical care rotations, of which at least 8 weeks must occur at the PGY-2 level or above (Core)
EMRA opposes this change.
EMRA believes ED management of a critical patient is very different from ICU management of a critical patient, and that ICU experience is not a substitute for critical ED patients. We highlight our comments on 1.8.j where we recommend a required minimum number of critical care patient encounters (180). Adopting a required number of encounters would eliminate the need for this requirement.
Return to TopRequirement 4.11.d.3.d
When the aggregated critical care volumes in the emergency departments across the primary and participating sites do not total at least 120 critical care patients per approved resident position in the program, a minimum of at least four weeks of additional critical care experience must be added to the curriculum. (Core)
EMRA opposes this change.
EMRA believes ED management of a critical patient is very different from ICU management of a critical patient, and that ICU experience is not a substitute for critical ED patients. We highlight our comments on 1.8.j where we recommend a required minimum number of critical care patient encounters (180). Adopting a required number of encounters would eliminate the need for this requirement.
Return to TopRequirement 4.11.d.4
At least 24 weeks, or the equivalent, must be dedicated to the care of neonates, infants, and children. The time is calculated by summing identified rotations and equivalent months. (Core)
EMRA supports this change with amendments.
EMRA supports the overall requirement for 24 weeks, or the equivalent, to be dedicated to pediatrics. However, we recommend increasing the Pediatrics Emergency Department time to 18 weeks and requiring a minimum of 1,000 pediatric patient encounters throughout residency.
Our suggested structure would be the following:
- At least 24 weeks, or the equivalent, must be dedicated to the care of neonates, infants, and children.
- At least 18 weeks, or the equivalent, must occur in an Emergency Department and total at least 1000 patient encounters.
- At least 4 weeks must occur in an ICU.
- At least 2 weeks must occur in the Pediatric ICU
For reference, averaging 45 hours/week for 18 weeks would give residents 810 hours in the Peds ED. To reach 1,000 patient encounters they would need to average 1.23 patients/hour.
Return to TopRequirement 4.11.d.5
Residents must have at least a 2-week experience in obstetrics. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.d.6
Residents must have at least a 2-week experience in administration/quality assurance. (Core)
EMRA opposes this change.
We recommend Admin/QA be a structured experience. We agree that Administration and QA are important topics for programs to cover in training but do not think they require a discrete time mandate. Many programs already accomplish this in a longitudinal co-curricular fashion and mandating a time component could hinder curriculum creativity and optimization, which is why we think it would be better as a structured experience.
Return to TopRequirement 4.11.d.7
Residents must have at least a 2-week experience in toxicology, including experience in addiction medicine/substance use disorder. (Core)
EMRA opposes this change.
We recommend Toxicology and Addiction Medicine be a structured experience.
There is great variance in the number of Toxicology and Addiction Medicine cases among emergency departments. While some programs may benefit and/or need a rotation for these areas, many programs do not. Many emergency physicians encounter cases of addiction medicine/SUD on a daily basis, highlighting its nature as a core part of the practice of EM and the lack of need for a separate rotation.
Toxicology, on the other hand, is not prevalent enough to ensure that every resident could have a meaningful clinical rotation, though we support a structured experience for this as well. Two weeks on a Toxicology rotation would not guarantee any breadth of clinical experience.
Return to TopRequirement 4.11.d.8
Residents must have at least a 2-week experience in emergency medical services (EMS), including real-time medical control. (Core)
EMRA opposes this change.
We recommend EMS be a structured experience. We support the continued requirement for experience in EMS in a longitudinal fashion during residency without adding a discrete time requirement.
We also oppose the requirement for real-time medical control experience. Many programs will have opportunities for medical control experience while working an ED shift but do not think it should be required.
Return to TopRequirement 4.11.e.2
Removal of the stipulation that only 1 resident can be credited with the direction of each resuscitation and the performance of each procedure. (Core)
EMRA encourages clarification on this change.
This proposal is not unreasonable in and of itself, but we do request clarity on whether supervising a procedure counts toward performing a procedure.
Return to TopRequirement 4.11.f.4.a
Residents must have structured experience in non-laboratory diagnostics, including: performing and interpreting point-of-care diagnostic and procedural ultrasonography; (Core)
EMRA opposes this change.
We believe the requirements for ED-based bedside ultrasound procedures should be quantified. This skill is foundational to providing optimal emergency care, and repetition is key to developing competency with this modality. Further, when going through the credentialing process for jobs, employers are routinely asking for the specific number of ultrasounds performed.
Return to TopRequirement 4.11.f.5
Residents must have structured experience in telemedicine. (Detail)
EMRA opposes this change.
EMRA supports telemedicine training opportunities where available and appropriate. However, we believe that telemedicine is not yet prevalent enough for all programs to have the resources to ensure a high educational value of the structured experience.
Return to TopRequirement 4.11.f.6
Residents must have structured experience in primary assessment and decision-making for patients presenting with conditions that may also be treated by multidisciplinary teams responding to the emergency department (eg, STElevation Myocardial Infarction (STEMI), stroke, sepsis, trauma). (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.f.7
Residents must have structured experience in airway management, including intubation, airway adjuncts, surgical airway, mechanical ventilation, non-invasive ventilatory management, and ventilatory monitoring. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.f.8
Residents must have structured experience in ophthalmologic procedures, including slit lamp examination, lateral canthotomy/cantholysis, intraocular pressure measurement, and superficial foreign body removal. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.f.9
Residents must have structured experience in acute psychiatric emergencies, including management of agitation, de-escalation, the use and documentation of physical restraint and sedation, and suicide risk assessment. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.f.10
Residents must have structured experience in the performance of sensitive exams, including genitourinary exams. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.f.11
Residents must have structured experience in transfer and transitions of care to ensure appropriate patient disposition, including appropriate application of Emergency Medical Treatment and Labor Act (EMTALA) principles. (Core)
EMRA supports this change without comment.
Return to TopRequirement 4.11.f.12
Residents must have structured experience in observation medicine. (Core)
EMRA opposes this change.
EMRA supports experiences with observation medicine available to interested residents. While some departments do have ED observation units, observation medicine is not core to being an emergency physician, and thus, there should not be a mandated structured experience for it.
Return to TopRequirement 4.15.a
All residents must complete and disseminate a scholarly project. (Core)
EMRA supports this change without comment.
Return to TopRequirement 5.1.c.1
The program director must verify review each resident's records logs of major resuscitations and procedures to ensure the progress of each resident toward achieving competence as part of the semiannual evaluation. (Core)
EMRA supports this change without comment.
Return to TopRequirement 5.1.c.2
The program must address the well-being of residents, including informing them of available resources. (Core)
EMRA supports this change.
We support meaningful wellness initiatives but caution against any wellness assessment that could result in punitive measures.
Return to TopRequirement 5.1.e.1
An individualized performance improvement plan to remedy deficiencies must be discussed with the resident, in writing and on file. (Core)
EMRA supports this change.
We support a clear plan for improvement, clearly communicated to trainees at risk of requiring remediation.
Return to TopRequirement 5.1.e.1.a
Progress must be monitored and communicated with the resident at a minimum of every 3 months. (Core)
EMRA supports this change.
We support regular feedback for all residents, and especially for those who are at risk of requiring remediation.
Return to TopRequirement 5.1.f.1
Removal of the requirement that at least annually, each resident's competency in procedures and resuscitations must be formally evaluated by the program director. (Core)
EMRA supports this change, with caution.
We believe programs should regularly provide feedback specifically related to procedure and resuscitation numbers and competencies so that residents know if they are on track to meet requirements.
Return to TopRequirement 6.17.a.5
Residents must have a minimum of 1 day (24-hour period) free per each 7-day period, which cannot be averaged over a 4-week period. (Core)
Specialty-Specific Background and Intent: This 24-hour period will be free from at-home call, including sick call, jeopardy, or back-up call.
EMRA supports this change without comment.
Return to TopAdditional Feedback (Key Index Procedures)
Endotracheal Intubation
Procedural Sedation (adult)
Procedural Sedation (pediatric)
Pediatric Vascular Access
Intra-osseous Access
New Additions
EMRA opposes certain components of these proposed changes.
Endotracheal Intubation: EMRA believes there should be a required number of intubations performed specifically in the Emergency Department for familiarity with RSI and intubation of an unstable patient.
Procedural sedation: EMRA opposes the allowance of simulation for all procedural sedations. We think 10 adult and 10 pediatric sedations are low requirements and programs should not need simulation to provide these opportunities to their residents. We think that allowing simulation in this case would increase risk to future patients, which is an unnecessary risk given the high prevalence of procedural sedation.
Pediatric IV Access: We opposed a mandated number of Pediatric IV accesses. Pediatric IV access is not often a physician procedure.
IO Access: We oppose a mandated number of IO accesses. Unless at a trauma center, it is not a very common procedure, making the limited simulation allowance prohibitive. Additionally, we believe IO access is a very simple procedure that does not require reps to reach competence.
New Additions: EMRA recommends that lower acuity procedures such as laceration repairs and I&Ds have mandated minimums. This is in line with the acknowledgment that some residents are having less exposure to lower acuity areas of the ED.
Return to Top
Related Content
Apr 07, 2025
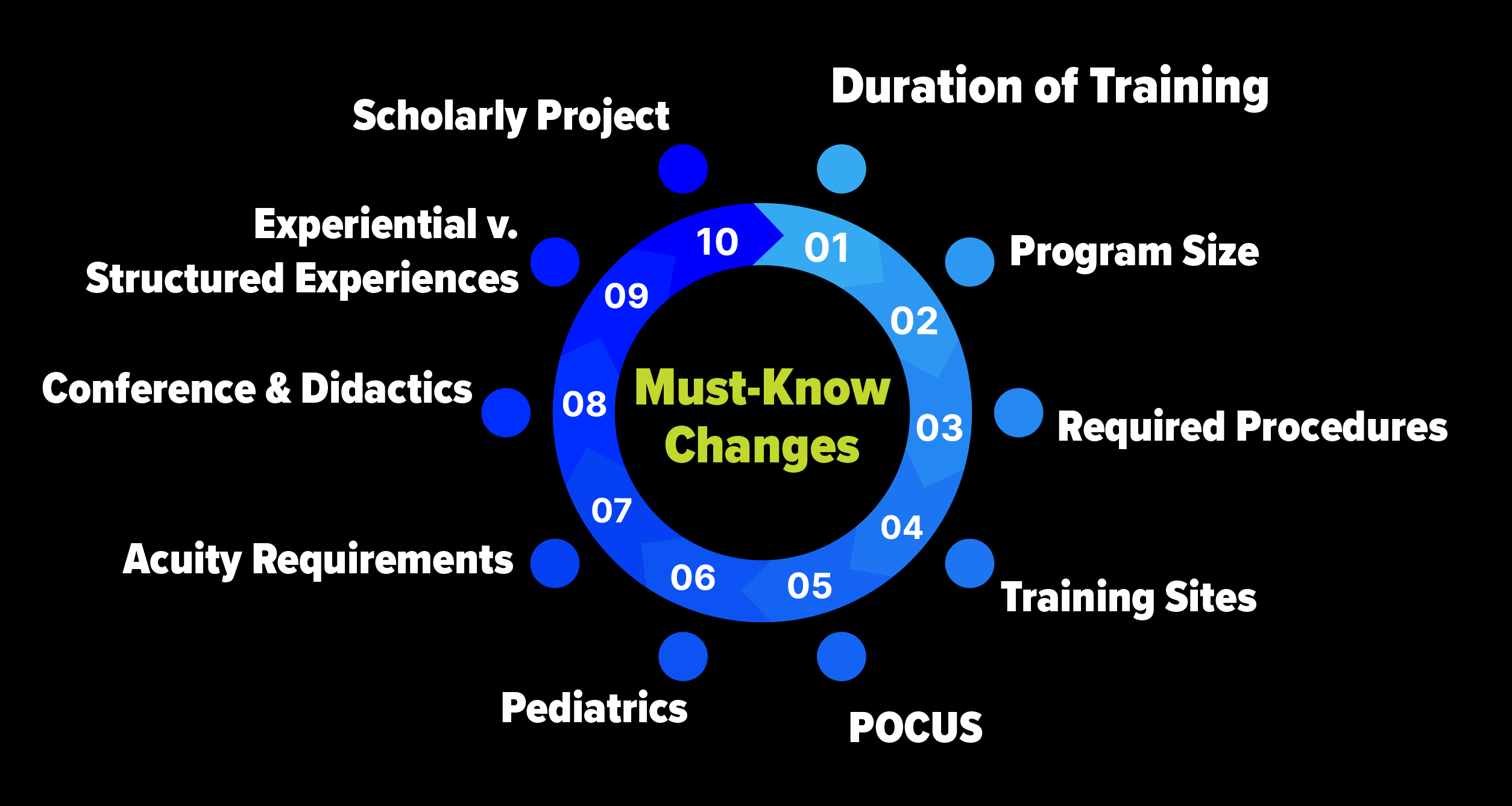
10 Must-Know Proposed Changes to Emergency Medicine Program Requirements from the ACGME
The EMRA Education Committee breaks down 10 key changes proposed by the ACGME Review Committee for Emergency Medicine. Public comments on the proposal will be accepted until May 1. EMRA urges you to understand the issues and make your voice heard with the ACGME.
Mar 31, 2025
ACGME Proposed Prog Requirements
The changes proposed by the ACGME would alter the training and careers of all future EM physicians. We share a belief that strong education helps residency graduates provide optimal care over the course of an optimal career. We're committed to that future.