ARDS Management ED and Beyond

ARDS Management ED and Beyond
June 15, 2020
EMRA*Cast host Dr. Alex Kaminsky takes a deep dive on the topic of Acute Respiratory Distress Syndrome (ARDS) with Dr. Sean Hickey and Dr. Evan Leibner.
Host
Alexander Kaminsky, MD
University of California San Francisco – Fresno
PGY4
@Alex_KamskyEM
EMRA*Cast Episodes
Guests
Sean Hickey, MD
Mt. Sinai Hospital, PGY-3
EMResident Articles
Overview:
Broad Strokes: ARDS is diffuse interstitial pulmonary edema secondary to increased pulmonary vasculature permeability. This causes a disruption in gas exchange.
More precise definition: Acute Respiratory Distress Syndrome (ARDS) is an acute diffuse, inflammatory lung injury, leading to increased pulmonary vascular permeability, increased lung weight, and loss of aerated lung tissue with hypoxemia and bilateral radiographic opacities, associated with increased venous admixture, increased physiological dead space and decreased lung compliance.
Etiology of injury pattern must be from a non-primary cardiopulmonary source.
Phases of Histologic Patterns:
Broad Strokes: Histologically in the lungs "diffuse alveolar damage" (DAD)
Initial response to injury:
Exudative phase, immune cell mediated damage to alveoli.
- Protein rich fluid buildup in the interstitium and alveoli.
- Inflammatory cytokines released leading to recruitment of macrophages/T-cells
-Any injury during this stage is worsened by stretch on alveoli by mechanical ventilation
Second phase is proliferative phase
- Beginning of healing process.
- Edema begins to be reabsorbed.
- Alveoli gradually regains integrity and function.
Third phase:
- Fibrotic phase
- Does not occur in all ARDS patients; linked with higher mortality
MOST COMMON CAUSES:
- Sepsis
- Aspiration (Hamman Rich Syndrome)
- Pneumonia
- Trauma
- Massive Transfusion
- TRALI
- Drug Overdose: ASA, Opioids, Cocaine,
- Pancreatitis
Diagnosis:
The Berlin Criteria
- Respiratory symptoms within ONE WEEK of clinical insult.
- Bilateral opacities on imaging – Not fully explained by effusion, lobar/lung collapse, or nodules.
- Respiratory Failure not fully explained by cardiac failure or volume overload. An objective assessment to rule out hydrostatic pulmonary edema is required. *
- A moderate to severe impairment of oxygenation is present while on >5 of PEEP
*Either objective assessment (echo) which excludes hydrostatic edema, or risk factors for ARDS (sepsis, pancreatitis, trauma, pneumonia).
Primary Literature:
- The ARDS Definition Task Force*. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA. 2012;307(23):2526–2533. doi:10.1001/jama.2012.5669
- Fan E, Brodie D, Slutsky AS. Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment. JAMA. 2018;319(7):698‐710. doi:10.1001/jama.2017.21907
Evaluation of Oxygenation: The P:F Ratio
- PaO2/FiO2 ratio is the ratio of arterial oxygen partial pressure to fractional inspired oxygen
- At sea level normal is > 500mmHg
- Mild ARDS: PF 200-300
- Moderate ARDS: PF 100-200
- Severe ARDS: PF < 100
Can be used as a rough guide to whether there is a significant A-a gradient present.
PaO2 should = FiO2 x 500 (e.g. 0.21 x 500 = 105 mmHg)
Treatment
Mild ARDS (PF 200-300): Consider BiPAP in patients who are awake, alert, protecting their airway and oxygenating/ventilating.
Majority Will Require Mechanical Ventilation
Key Point: Goal is to optimize gas exchange, but avoid barotrauma, volutrauma, atelectotrauma and biotrauma. This is accomplished by low tidal volumes and dry volume status as tolerated.
ARDSnet and Clinical Considerations
http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf
http://www.ardsnet.org/studies.shtml
- Tidal Volumes at 4-6ml/kg of IDEAL body weight.
Pro-tip from Evan: Pick your ideal vent mode based on comfort. There are lots of fancy and potentially optimal ventilator modes, such as Bi-level, oscillatory modes, and otherwise. Unfortunately, these are nuanced and can leave to harmful outcomes if doctors and RT’s are not intimately familiar.
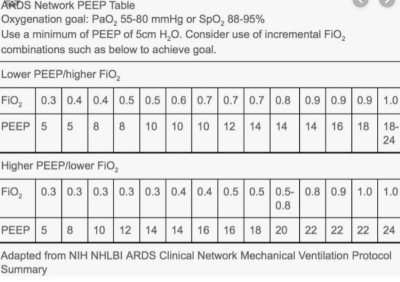
2. High vs low PEEP tables have not been shown to affect mortality. Must be careful as high PEEP can reduce cardiac output.
3. To maintain the minute ventilation with LTV you must increase the RR.
However, by increasing the RR too much you can cause auto-PEEP. Thus, permissive hypercapnia can be tolerated unless acidotic (pH <7.15)
- Auto-PEEP can be measured by measuring the pressure during an expiratory hold and calculating by subtracting the provided PEEP by the total pressure.
- Maintain plateau pressures below 30. This reduces the amount of volotrauma on patients. Can be accomplished by providing an inspiratory hold and measuring the pressure.
- Maintain driving pressure below 15. It has been shown to improve mortality. Most likely reduces atelectotrauma.
Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55.
- Keep patients DRY – Early pressers as needed. The FACTT trial targeted a CVP <4 lead to an improvement in ventilator free days, an improvement in oxygenation index, less time in the ICU without an increase in shock.
Wiedemann HP, et al. "Comparison of two fluid-management strategies in acute lung injury". The New England Journal of Medicine. 2006. 354(24):2564-75.
- Consider paralyzing patients with long-acting paralytics (cisatracurium) if desynchrony with the ventilator. The ROSE trial showed no benefit, this is controversial and still a practice by some intensivists.
National Heart, Lung, and Blood Institute PETAL Clinical Trials Network. "Early neuromuscular blockade in the acute respiratory distress syndrome". The New England Journal of Medicine. 2019. 380(21):1997-2008.
- Can consider APRV which was shown by Zhou et al to improve mortality.
APRV: Essentially a persistent inspiratory phase by ventilator, with “exhallation” phase where the vent triggers “off.” To allow for passive exhalation. Theory is it keeps alveoli open for longer to participate in recruitment and gas exchange and then gives longs a “break.”
https://emcrit.org/squirt/aprv/
- Traditional recruitment maneuvers do not improve mortality according to the ART trial.
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA. 2017;318(14):1335–1345. doi:10.1001/jama.2017.14171
- Proning patients substantially improves mortality. Increased recruitment of atelectatic lung according to the Proseva trial
Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159‐2168. doi:10.1056/NEJMoa1214103
- Consider EARLY for VV-ECMO. ECMO is believed to be potentially a cost-effective measure that increases survival without severe disability at 6 months in patient with severe ARDS. CESAR trial.
Especially Consider if single organ system is affected in otherwise non-terminal patients
Peek GJ, et al. "Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicentre randomised controlled trial.". The Lancet. 2009. 374(9698):1351-1363.




