ARTICLE: Trummer G, Benk C, Pooth JS, et al. for the Extracorporeal Multi-Organ Repair Study Group. Treatment of refractory cardiac arrest by controlled reperfusion of the whole body: a multicenter, prospective observational study. J Clin Med. 2023;13(1):56.
- Notable review: RACC Lit Review. EMCrit. Feb. 2024. Available to subscribers.
OBJECTIVE
To be the first prospective observational study to test improvements of outcomes and organ function after prolonged cardiac arrest using a new ECMO technology called controlled automated reperfusion of the whole body
BACKGROUND
Sudden cardiac arrest (CA) is one of the leading causes of mortality worldwide. These are typically broken down into out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA) with low survival rates of <10% and <14% respectively.1,2 Extracorporeal membrane oxygenation (ECMO), has shown potential at improving survival rates over traditional conventional cardiopulmonary resuscitation (CCPR) for both OHCA and IHCA.3 ECPR is the placement of an individual experiencing cardiac arrest onto ECMO as a bridge to definitive management of the underlying precursor to the cardiac arrest. Unfortunately, ECPR has not generated consistent results in multiple randomized control trials. Furthermore, this technology has primarily focused on shockable cardiac arrest, which has significantly more favorable outcomes and represents only a portion of CA.4
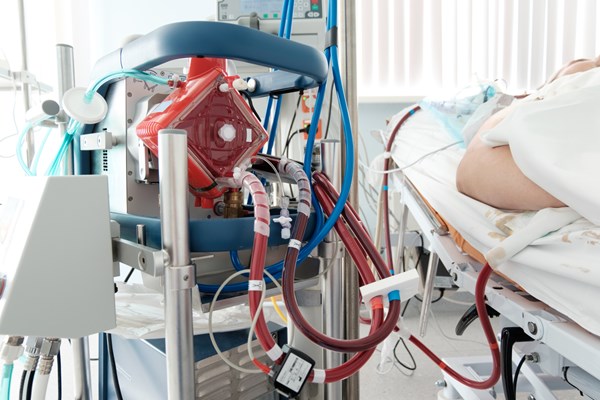
Typical ECMO involves equipment that allows one to “bypass” heart and lung function. A simplified summary of this includes a venous cannula to pull deoxygenated blood from the body, a centrifugal pump to move the blood, heat exchangers to control temperature, an oxygenator to provide oxygen and remove CO2, and an arterial cannula to return blood. Typical parameters controlled are flow, oxygen, and sweep gas rate.5
A new ECPR technology called “controlled reperfusion of the whole body” (CARL) has been developed. This ECPR circuit attempts to use multimodal therapy and controls to address the specific pathophysiology unique to cardiac arrest and prolonged CCPR. Key differences from traditional ECPR technology includes: pulsatile blood flow, adjustment of 14 blood parameters (eg, oxygen, free radicals, calcium, magnesium, etc.), cytoprotective perfusate prime solution, real-time monitoring and manipulation of hemodynamic, metabolic, and temperature parameters, and a physically more mobile device for OHCA. This technology has recently been tested and used by multiple hospitals with case reports and a case series published.6
This is a prospective multicenter observational study that looks at outcomes in cardiac arrest with CARL ECPR technology. This study includes shockable and nonshockable rhythms in OHCA and IHCA. This is a key difference as previous ECPR studies have primarily focused on refractory shockable rhythm CA. In addition, the hemodynamic and metabolic parameter criteria to place a patient on CARL were significantly lower than current “traditional” guidelines currently suggested for ECPR application. In summary, this study using CARL looks at outcomes for a new ECPR technology in a wide variety of patients experiencing CA.
DESIGN
This was a multicenter, international, prospective, non-interventional, open, single-arm study. This was an “all-comers” study meaning there were no formalized inclusion criteria. Patients were included regardless of age, duration of CCPR, transport time, and initial rhythm. The decision to cannulate the patient was made if the patient had refractory cardiac arrest with no ROSC, and was deemed to be an appropriate candidate by the cannulating physician based on currently accepted guidelines, and generally accepted indications and contraindications for ECPR.
Patients were cannulated with conventional femoral arterial and venous cannulation. Following cannulation, the CARL controller was connected and started. As above, this uses real-time monitoring of several parameters to deliver personalized treatment for multi-organ failure. After transport, patients were generally treated for at least several days in an intensive care unit. Further details of the ECPR and CARL operation can be found in the article's supplemental material. The study later discusses results compared to a historical control group using ECPR data from their own institutions.
INCLUSION CRITERIA
- As this was a non-interventional study, currently accepted indications/contraindications were used to decide eligibility. The decision to cannulate was ultimately made by the treating physician.
EXCLUSION CRITERIA
General contraindications for ECPR/CARL:
- Established Patient DNR order
- Stable ROSC upon arrival of the cannulation team
- Inability to cannulate femoral vessels
- Septic shock
- Known pre-existing severe neurologic impairment
- Known diagnosis of end-stage malignancy
- Inability to achieve the minimal standards of extracorporeal perfusion such as: appropriate flow, pressures, and/or multi-organ protection
PRIMARY OUTCOME
- Overall survival at hospital discharge
- A good neurologic outcome at hospital discharge as defined as a CPC score of ≤ 2
SECONDARY OUTCOME
- Non-cerebral bleeding: defined as any bleeding requiring intervention such as transfusion or surgical intervention.
- Cerebral bleeding–confirmed on CT imaging. All cerebral bleeding was included regardless of size, location, or clinical implication.
- Successful arterial and venous cannulation
- Controlled Oxygenation of at least 100-200 mmHg
- Pulsatile flow: the automated generation of a pulsatile flow was documented in CARL controller datasheet
- Target PaCO2 of 40-45 mmHg
- Target pH in the first 30 min <7.25, and then 7.35-7.45 following initial 30 min
- Target MAP 60-100
- Mild systemic hypothermia: 32-33°C
- Kidney function and need for RRT
- Acute kidney injury defined as creatinine increase 1.5 x baseline or increase of > 26.3 μmol / 0.3 mg/dL within 48 hours
- Liver function: measured by the enzyme levels of AST/ALT
- Pulmonary function: measured by blood gas and the need for mechanical ventilation
- Cardiac and hemodynamic functions: these were semi-quantitatively assessed by documentation of inotropic agent use in the patient's chart. Assessment of inotrope use at days 1, and 7, or of either CARL or ECLS termination, at day 30 and at hospital discharge
- Presence of infections: this was registered if proof via microbiological culture or laboratory values were obtained.
- Duration (in hours) of controlled automated reperfusion of the whole body
- Duration of ICU stay in hours
- Duration of hospital stay (in days): Time in hospital between admission (for OHCA) or occurrence of CA (for IHCA) and release from any hospital treatment
KEY DEMOGRAPHICS
- The final cohort included 69 patients who experienced CA and were placed on CARL
- IHCA occurred in 42% of patients. OHCA occurred in 58% of patients, of these, 35% (14/40) were cannulated outside of the hospital.
- 8 patients (12%) with unwitnessed CA were included
- An initial shockable rhythm was seen in 53% of patients with the remainder in an initial non-shockable rhythm.
- The severity of both no, and low-flow, time (CA and CCPR) was reflected by the mean pH (7.0 ± 0.3), and median lactate of 10.1 (7.7 -- 12.3) before the start of extracorporeal circulation.
- 9 patients included had essentially “non-survivable” disease leading up to CA
KEY OUTCOMES
- Overall survival at hospital discharge: 42.0%.
- 3% excluding patients with “non-survivable” causes of CA
- Favorable neurologic outcomes:
- CPC 1 + 2 in surviving patients at 90 days was 79.3% (23/29)
- Of the entire cohort, CPC 1 + 2 survival was 33%
- The most favorable survival outcomes were noted in the IHCA patients (51.7%) and in the OHCA patients who were cannulated out-of-hospital (57.1%).
- CCPR duration ≤ 30 min and age of 18–64 years were associated with 100% survival.
- CCPR ≥ 60 min and age ≥ 75 years were associated with 0% survival.
- Patients aged 65–75 years demonstrated satisfactory survival rates across different CCPR durations (≤30 min (50%), 30–60 min (40%), and ≥60 min (29%)).
- All 4 patients aged > 75 years survived when the CCPR duration was ≤30 min
SECONDARY OUTCOMES
- Primary cause of death was either neurological (25%) or multi-organ failure (27.5%).
- Median duration of stay in the ICU was 8.1 days, 28 days for surviving patients
- The duration of CCPR (low flow) for OHCA was 68.5 min and for IHCA patients 33.5 min.
- CCPR duration was ≥30 min for 74% of all patients and >60 min for 55%.
- In the OHCA group, 61% had a CCPR duration of ≥60 min.
- Time needed to establish extracorporeal circulation was ≤15 min for 56% and ≤20 min for 71%.
- Of survivors, only one required RRT, and none required any form of mechanical circulatory support at the point of hospital discharge
- A full list of the secondary outcomes can be found in the article's supplemental data.
LIMITATIONS
- This study has limitations inherent to all observational studies including: small sample size, lack of randomization, inability for blinding, and lack of a control group.
- The comparison group was a composite of institutional ECPR results, published registries and three previous randomized trials.
- Potential selection bias and lack of generalizability due to location-specific patient populations, EMS systems, center experience with ECPR, and patient selection criteria.
- Adherence to the study protocols varied among centers. Potential center-specific differences were not explored in this study.
- The COVID-19 pandemic occurred mid-study and caused reallocation of resources, decreased participant recruitment, and potentially had effects on the survival of OHCA
- This study did not enforce strict inclusion and exclusion criteria similar to previous ECPR studies but instead included a wide variance in CA patients. Future studies may implement strict criteria allowing a more direct comparison to previous ECPR studies.
EM TAKE-AWAYS
ECPR continues to show promising results for patients undergoing cardiac arrest. CARL technology implements a new design that provides comprehensive monitoring and multimodal therapy to address the unique pathophysiology of cardiac arrest. This study is the first multicenter observational study using CARL technology and shows impressive survival rates for both non-shockable and shockable rhythms in cardiac arrest. This is a large difference from almost all previous ECPR studies. Further trials are needed, but these exciting results should spur further research with CARL technology for ECPR.
REFERENCES
- Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE. One-year survival after in-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2018;132:90-100.
- Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61.
- Klee TE, Kern KB. A review of ECMO for cardiac arrest. Resusc Plus. 2021;5:100083.
- Yannopoulos D, Bartos J, Raveendran G, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396(10265):1807-1816.
- Lequier L, Horton SB, McMullan DM, Bartlett RH. Extracorporeal membrane oxygenation circuitry. Pediatr Crit Care Med. 2013;14(5 Suppl 1):S7-S12.
- Philipp A, Pooth JS, Benk C, Mueller T, Lunz D. Enabling the control of reperfusion parameters in out-of-hospital cardiac arrest: First applications of the CARL system. Perfusion. 2023;38(2):436-439.
- Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association [published correction appears in Circulation. 2023 Feb 21;147(8):e622] [published correction appears in Circulation. 2023;148(4):e4]. Circulation. 2023;147(8):e93-e621.