The patient, a 53-year-old male, has past medical history notable for lung cancer, right lung pneumonectomy approximately one year ago, and recent bronchoscopy three days prior to ED arrival.
He presented to the emergency department with sudden-onset severe shortness of breath immediately prior to arrival. In the ED, the patient was visibly tachypneic, diaphoretic, anxious, using accessory muscles of respiration, and appeared to be rapidly compensating toward extremis.
Explanation
Left-sided tension pneumothorax with history of remote right pneumonectomy. Our initial differential diagnosis included upper respiratory compromise (e.g., epiglottis or internal obstruction due to recent procedure), tension pneumothorax, post‐pneumonectomy syndrome (PPS), flash pulmonary edema, cardiac tamponade, ACS, and less likely DKA or anaphylaxis.
On portable chest X-ray outside of the patient’s room, the patient was noted to have a left-sided pneumothorax in his remaining lung with tracheal deviation to the right. In the context of rapid decompensation, a 14-gauge needle was placed in the left anterior third intercostal space, which temporized the patient. Subsequently, a 14-French chest tube was placed in the patient’s midaxillary line on the left side, with immediate improvement of hemodynamics, tachycardia, and respiratory rate. The patient was admitted to thoracic surgery service and was doing well approximately three months out without pneumothorax recurrence.
Image 1
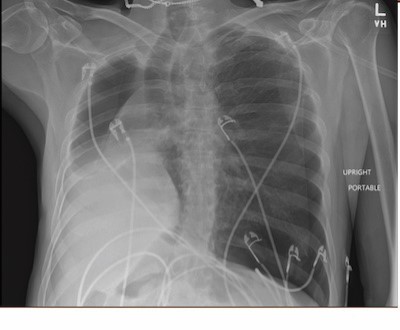
Image 2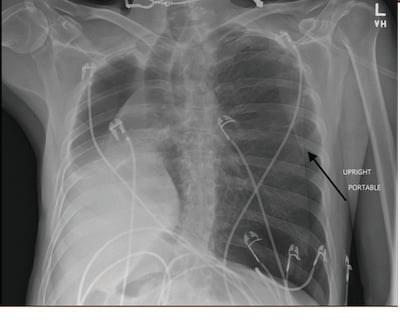
Description
The leading cause of iatrogenic pneumothorax is transthoracic needle aspiration, though in this case, pneumothorax was most likely due to transbronchial lung biopsy two days prior to presentation.1 Although this patient had a tension pneumothorax, it is worth noting that post‐pneumonectomy syndrome (PPS) is a rare post-pneumonectomy complication occurring typically within several months and caused by excessive mediastinal shifting that results in airway compression.2
References
- McKnight CL, Burns B. Pneumothorax. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441885/
- Jung JJ, Cho JH, Kim HK, et al. Management of post-pneumonectomy syndrome using tissue expanders. Thorac Cancer. 2016;7(1):88-93. doi:10.1111/1759-7714.12282



