This article aims to provide a standardized approach to assessing diving-related injuries.
We’ll first review the unique aspects of a history critical to diagnosing diving-related injuries. We’ll then present two very general chief complaints and work through a list of differentials to consider, each associated with a specific phase of a dive.
Dive Injury HPI
The primary survey should be the first evaluation point for any critically ill dive casualty. Once complete, a focused dive-related history is imperative. For any diving-related complaint, the following component-based HPI questions can help narrow the differential:
Timing
- When did the symptoms begin? (The highest yield question of the HPI)
- Descent, bottom, ascent, or after the dive?
- If after, how long after?
Profile
- Maximum depth
- Time spent at depth
- Number of dives during the day
- Surface interval between dives
- What type of activity/work was performed while diving?
- Did the ascent occur at a standard rate?
- What gas mixture and equipment were used? (Commonly referred to as dive “rig”)
- Where were the tanks pressurized?
Additional Information:
- Did any other divers have symptoms?
- What activities occurred after diving?
- Was there an ascent to altitude by aircraft or mountainous terrain after the dive?
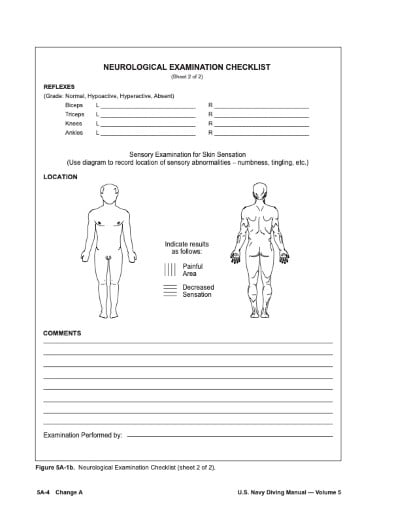
Additionally, any diving-related chief complaint should include thorough neurologic and pulmonary physical exams.
The U.S. Navy utilizes a standardized guide to assist in the initial evaluation of diving-related injuries. Although not specifically designed for medical personnel, it will greatly assist those who do not encounter diving injuries frequently.
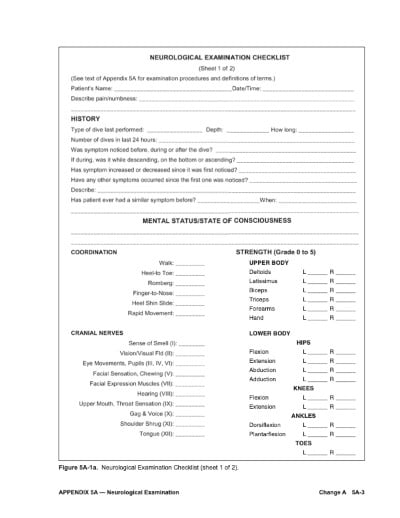
US Navy Figure 5A-1a, Neurological Examination Checklist9
US Navy Figure 5A-1a, Neurological Examination Checklist9
Case 1
Neurologic Presentation: Dizziness
A diver presents to your emergency department with a neurologic complaint. In this case, we’ll use dizziness as it can be seen in almost every one of the following differentials. Other concerning complaints in the neurologic category could include altered mental status or a focal neurologic deficit. The following is a list of differentials to consider, grouped by stage of the dive.
Descent
The differential for a diver experiencing dizziness during descent is limited. A simple cause may be caloric vertigo, which occurs when cold water enters the ear unilaterally and stimulates the vestibular system. The temperature inequality may be caused by hoods or earplugs that alter the normal flow of cold water into the outer ear. This condition is transient and self-limited.
Ear barotrauma comes in two forms, the much more common middle ear barotrauma and the less common inner ear barotrauma. In both conditions, an inability to equalize the middle ear air space during descent leads to significant negative pressure in relation to the outside environment resulting in distortion and damage to tissues. The tympanic membrane (TM) is most commonly damaged. This damage initially presents as pain and bleeding within the layers of the TM and may lead to rupture. Divers can experience vertigo and hearing loss after TM rupture. Discontinuation of the dive and cessation of diving until the TM heals is recommended. The same mechanism causes inner ear barotrauma, but the damage is to the round or oval windows of the inner ear. This disruption can cause a leakage of endolymph from the inner ear. Symptoms include severe vertigo, nausea/vomiting, and hearing loss.2Referral to ENT is recommended for patients who sustain inner ear barotrauma.
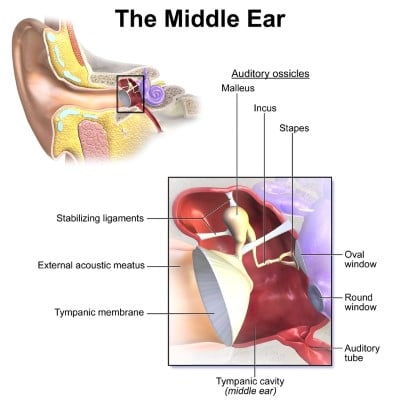
Ear Anatomy, Middle Ear10 (From Wikimedia Commons, the free media repository. File: Blausen 0330 EarAnatomy MiddleEar.)
Bottom
Dalton’s Law of Partial Pressures states that the partial pressure of any gas is the product of the percentage of that gas in the mixture multiplied by the depth. At sea level, atmospheric pressure is 1 atmosphere (ata). Oxygen is 21% at sea level, therefore ppO2 at sea level = 0.21 ata. In seawater, every 33 feet of depth adds an additional atmosphere of pressure. Thus, the partial pressure of oxygen in a standard air mixture at 66 feet is calculated below:
66 ft/33= 2 atm
2 atm +1 ata (1 ata @ sea level)= 3 ata
0.21 FiO2 X 3 ata= 0.63 ata ppO2
Atm represents the number of atmospheres measured over surface pressure. Ata presents absolute atmospheres, which includes the pressure from the atmosphere above our heads at sea level. This concept is important because the effects of any gas are directly related to its partial pressure.
The bottom phase of the dive presents a set of new differentials. We’ll start with incorrect gas mixtures. Hypoxia would likely begin to manifest a few minutes into a dive when the diver first reaches the bottom. Hypoxia can occur in rebreather diving, where exhaled air rich in CO2 and low in O2 is recycled within the diving rig using a chemical-based scrubbing system to remove the CO2 and an oxygen source to add additional oxygen. Improper addition of oxygen to the gas mixture by the rig can rapidly lead to hypoxia. Hypoxia can also occur in self-contained underwater breathing apparatus (SCUBA) or surface-supplied diving when gasses are mixed incorrectly. In both SCUBA and surface-supplied diving, exhaled gasses are released from the rig and into the water as bubbles. Low percentages of oxygen are used when diving to extreme depths. For example, a 3% oxygen mixture could be used when diving to depths of around 200 feet. This mixture would lead to a ppO2 of approximately .21 ata (.03 FiO2 x 7 ata [198ft] =.21 ata O2), equal to surface air. However, using that gas mixture at a depth of 66ft would be deadly as the ppO2 would only be .09 ata (.03 FiO2 x 3 ata =.09 ata O2), essentially equivalent to breathing 9% oxygen at the surface. The primary mechanism driving respiration is carbon dioxide. Low oxygen alone does not provide a robust respiratory drive; thus, hypoxia commonly presents late as confusion, dizziness, or nausea. Treatment is simple: Provide more oxygen!
Carbon monoxide (CO) poisoning is also likely to manifest during this period. CO poisoning may be caused by gas bottles pressurized with a petroleum-based fuel-burning air compressor. If the air being compressed into a tank is in close proximity to the exhaust of the compression system, CO will be pressurized into the air canister. Like all other gasses, the partial pressure of CO is multiplied by depth. CO poisoning commonly presents with headaches, nausea, vomiting, confusion, or lethargy. CO monoxide is treated with 100% oxygen, and hyperbaric therapy is indicated in patients with a CO > 25% or 20% if pregnant, loss of consciousness, severe metabolic acidosis (pH <7.1), or evidence of end-organ ischemia.3 A Navy Treatment Table 6 is recommended.1
As depth surpasses 100 ft, or more specifically, as the partial pressure of nitrogen exceeds 4 ata, the risk of nitrogen narcosis increases. Nitrogen at high partial pressures has a narcotic effect, simulating drug or alcohol intoxication. Divers expecting to dive to significant depths generally use helium instead of oxygen, as helium does not have the same narcotic effects as nitrogen. Nitrogen narcosis manifests as giddiness, poor decision-making, loss of skill, tingling, inappropriate laughter, and lack of concern for safety. Nitrogen narcosis in itself is not dangerous, but divers can quickly become tangled or lose their air source in their confusion. There are sea stories of divers cutting their own air lines due to the narcotic effect of nitrogen. Treatment is simple: Ascent to a shallower depth rapidly corrects the problem with no sequelae.
CNS oxygen toxicity is another condition with which risk increases with increasing depth. High partial pressures of oxygen have a toxic effect on the central nervous system. CNS oxygen toxicity occurs at partial pressures of Oxygen over 1.3 ata (USN) -1.4 ata (PADI).1,4 For a diver breathing air, oxygen toxicity would not be a risk until a diver reached 187 ft. However, divers breathing NITROX or another form of mixed gas, oxygen toxicity can occur at much shallower depths. A commonly used NITROX mixture in recreational diving is 32% oxygen. With this mixture, a diver would reach a ppO2 of 1.4 ata at 111ft. Oxygen toxicity presents as a group of possible symptoms known as VENTID-C. This acronym stands for visual symptoms (tunnel vision or blurry vision), ear symptoms (tinnitus), nausea, vomiting, twitching and tingling, irritability, dizziness, and convulsions.1 O2 toxicity is easily treated by ascent to a shallower depth, although aborting the dive is recommended. The most significant risk with CNS O2 toxicity is convulsions, which could quickly lead to drowning.
Ascent/Post Dive
Decompression sickness (DCS), also known as “the bends,” and arterial gas embolisms (AGE) are the most common injuries during ascent or after a dive. We’ll cover arterial gas embolism first as it is more likely to occur chronologically before DCS. An AGE occurs due to overexpansion of gas in the lungs, a result of Boyle’s Law. Boyle’s law states that the pressure and volume of a gas are inversely related. As a diver ascends to the surface, air-filled structures throughout the body will expand (lungs, sinuses, middle ear, dental cavities). Rapid ascent with a closed glottis does not allow expanding air in the lungs to escape. This air must go somewhere, which can result in mediastinal emphysema, pneumothorax, or subcutaneous emphysema, listed in descending order of likelihood. These injuries are collectively known as pulmonary overinflation syndrome (POIS). This damage can also result in air bubbles directly entering the arterial system, leading to deadly consequences. These bubbles rise against gravity through the arterial vascular system to the most superior portion of the body, the brain. Once these gas emboli lodge in smaller arterioles, they cause damage similar to thrombotic clots, preventing blood flow and damaging endothelium. AGEs present within the first 10 minutes of surfacing from a dive and are an immediate emergency. AGEs present with a wide range of symptoms related to the location of the brain in which they damage and can present as severely as immediate unconsciousness upon surfacing. When symptoms correlate with both AGE and DCS, if they develop within ten minutes of ascent, they are treated as AGE until proven otherwise. Treatment is recompression with Navy Treatment Table 6.1
Decompression sickness results from the rules of Henry’s Law. This law states that the amount of dissolved gas in a liquid is proportional to its partial pressure above the liquid. In diving, the human body can be substituted for the liquid mentioned above. As a diver descends deeper, more of whatever gas mixture they breathe will dissolve in their tissues. This becomes more of a problem on ascent, as the diver’s tissues have a saturation point directly related to depth. If a diver ascends too quickly after a long dive, the amount of gas dissolved in their tissues becomes greater than the maximum saturation point, and the gas bubbles out of solution. DCS is further categorized into two types, DCS Type I, in which involvement is limited to a single joint, the skin, or the lymph system, and DCS Type II, which can involve the nervous system, inner ear, or pulmonary system. Gas bubbles formed in DCS are generally caused by helium or nitrogen since these gasses are inert and cannot be metabolized. The body can metabolize and break down oxygen, so it is less likely to cause issues, even if it exceeds its saturation point.
DCS can cause neurologic symptoms through several different mechanisms. Direct or “de novo” formation of bubbles within the tissues of the brain or spinal cord will cause local damage to these organs. Symptoms will be directly related to the structure in which the bubbles are found. Neurologic DCS has a predilection for the spinal cord, leading to paresthesias, paralysis, incontinence, or any number of peripheral neurologic complaints.5
Bubbles from decompression sickness can also occur in the venous system and are known as venous gas emboli or VGEs. VGEs can cross through cardiac or pulmonary shunts to the arterial system. At this point, they become AGEs and can have all of the effects of previously discussed AGEs. However, the term AGE in diving medicine is almost always used to describe AGEs caused by pulmonary overinflation. MRI can locate ischemia and edema from DCS in both the brain and spinal cord, but obtaining advanced imaging should not delay treatment.
The final neurologic possibility resulting from DCS is that of inner ear DCS. This is a relatively rare cause of DCS, more likely to be seen in saturation divers breathing helium. In inner ear DCS, bubbles form de novo in the inner ear structures, leading to dizziness similar to that of an otolith. Of course, immediate differentiation between inner ear DCS and central intracranial DCS is challenging. Still, EM physicians should utilize the same strategy for differentiating central versus peripheral vertigo symptoms in non-diving patients, with a diving history leading to consideration of inner ear DCS as an additional peripheral cause.
All patients with neurologic, pulmonary, or inner ear DCS should be treated with a Navy Treatment Table 6,1 with neurology follow-up. For both AGE and DCS, supplemental oxygen should be initiated as soon as possible if a recompression chamber is not immediately available.
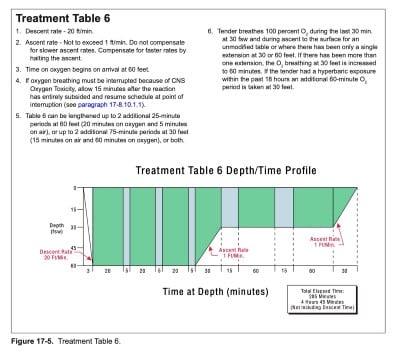
Treatment Table 61
It is important to note that while we typically associate the bubbles of DCS with occlusive mechanisms associated with the presentation of an ischemic cerebrovascular accident, DCS symptoms do not always localize to a specific neurologic legion or territorial infarct. Newer research is beginning to shed light on the multifaceted etiology of DCS, with bubble vascular occlusion not being the only element of the complex presentation.6,7
Alternobaric vertigo can cause vertigo or dizziness during ascent, although it can also occur during descent. The mechanism involved is an imbalance in pressures between the middle ear spaces. On ascent, the middle ear pressures increase, and the eustachian tube releases this excess gas into the nasopharynx. A pressure imbalance is created if one of these tubes is blocked. Treatment is to attempt the diver’s preferred equalization strategy and ascend slowly.
Case 2
Cardiopulmonary Presentation: Shortness of breath
The next diving-related chief complaint that emergency physicians should be familiar with is shortness of breath and/or chest pain.
Descent/Bottom
A diver experiencing shortness of breath early in a dive may be suffering from hypercapnia. As discussed earlier, CO2is the primary driver of respiration, and elevated levels of CO2 will consistently result in an increased respiratory rate and feelings of dyspnea. Hypercapnia is less likely to occur with SCUBA divers, as it would be challenging to contaminate a SCUBA bottle with high levels of CO2. It can happen in rebreather diving if the rig is not functioning correctly or if the CO2 absorbent is no longer pulling CO2 from the system as it should. Hypercapnia can also occur when diving with full face mask or hard hat systems, as these devices include areas of stagnant air or dead spots, which allow for the build-up of CO2 in a localized area. This problem can easily be remedied by venting the space with fresh gas. Elevated CO2 also increases the risk of CNS oxygen toxicity, has an additive effect with nitrogen narcosis, and may increase DCS risk.
Diving with a rebreather poses additional risks as the chemicals used to scrub CO2 are highly toxic when they come into contact with water. Ingestion of these caustic alkaline chemicals, known as a caustic cocktail, can lead to severe damage to the airway. Symptoms include choking, gagging, foul taste, and burning. Initial management should include a fresh water rinse of the mouth. These patients may require intubation, decontamination, bronchoscopy, and endoscopy.
Ascent/Post Dive
As discussed in the section on AGEs, overexpansion of air in the lungs forces gas into nearby structures. Thus, pneumothorax (PTX) should be considered in any patient with chest pain or SOB. If a concurrent diving injury requiring recompression is present, a PTX should be addressed before the patient enters the recompression chamber. There is little risk with recompression, but during ascent in the chamber at the end of treatment, the air in pleural space will begin to expand again, causing further damage. Standard treatment for a PTX is appropriate to include needle decompression, chest tube, and inspired oxygen.
Pulmonary decompression sickness is colloquially referred to as “the chokes” and is the final form of Type II or emergent DCS we will discuss today. In the prior section, we discussed VGEs, which form de novo in the venous system in patients with DCS. In patients without a cardiopulmonary shunt, most of these gas emboli are filtered out of the vascular system by the lungs. Pulmonary DCS can occur in patients with an overwhelming burden of VGEs. Initial symptoms are cough, shortness of breath, burning substernal chest pain, pain with respirations, and increased respiratory rate. Radiographic findings are similar to that of pulmonary edema. Treatment is inspired oxygen, and a Navy Treatment Table 6.1
Conclusion
Although most diving-related injuries are not life-threatening, it is imperative to promptly establish contact with your on-call hyperbaric physician when a serious diving-related injury is identified. Your hyperbaric physician will guide you in your approach to treatment and may help you with the transportation of your patient to the nearest recompression chamber. If you do not have a readily accessible hyperbaric specialist, the Divers Alert Network (DAN) has a 24/7 hotline which you can contact at +1 (919) 684-9111. This number will connect you to a DAN medic who will further advise and help you locate the nearest recompression chamber.8
Finally, while we discussed in depth the differential diagnosis of diving injuries, divers also suffer from the same injury patterns as the general population. A diver who has multiple cardiac risk factors and presents with chest pain should be evaluated for acute coronary syndrome the same as every other patient with chest pain, with the diving injury differentials being considered in addition.
References
- Naval Sea Systems Command. U.S. Navy Diving Manual Revision 7. 2018;1(October 2011):Section 17-6.
- Inner Ear Barotrauma.
- Clardy, Peter; Manaker, Scott; Perry H. Carbon Monoxide Poisoning.
- Thalmann E. Oxygen Toxicity. Accessed August 1, 2022.
- Jallul S, Osman A, El-Masry W. Cerebro-spinal decompression sickness: report of two cases. Spinal Cord. 2007;45(1):116-120.
- Nossum V, Koteng S, Brubakk AO. Endothelial damage by bubbles in the pulmonary artery of the pig. Undersea Hyperb Med J Undersea Hyperb Med Soc Inc. 1999;26(1):1-8.
- Zhang K, Wang D, Jiang Z, Ning X, Buzzacott P, Xu W. Endothelial dysfunction correlates with decompression bubbles in rats. Sci Rep. 2016;6:33390.
- DAN Emergency Assistance. Accessed August 1, 2022.
- U.S. Navy Neurological Examination Checklist. From U.S. Navy Diving Manual. Distribution statement on cover page: “This document has been approved for public release and sale; its distribution is unlimited.”
- Blausen.com staff (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. (https://commons.wikimedia.org/wiki/File:Blausen_0330_EarAnatomy_MiddleEar.png), Blausen 0330 EarAnatomy MiddleEar, https://creativecommons.org/licenses/by/3.0/legalcode
https://en.wikipedia.org/wiki/Ear#/media/File:Blausen_0330_EarAnatomy_MiddleEar.png Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014.” WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436



