Case 1. The Patient
A 44-year-old male with a history of upper extremity DVT and MRSA positivity presents with a constant, throbbing left wrist and forearm pain. He denies any trauma to the affected extremity, and has no complaints of fevers, nausea, or recent illnesses. He has normal vital signs.
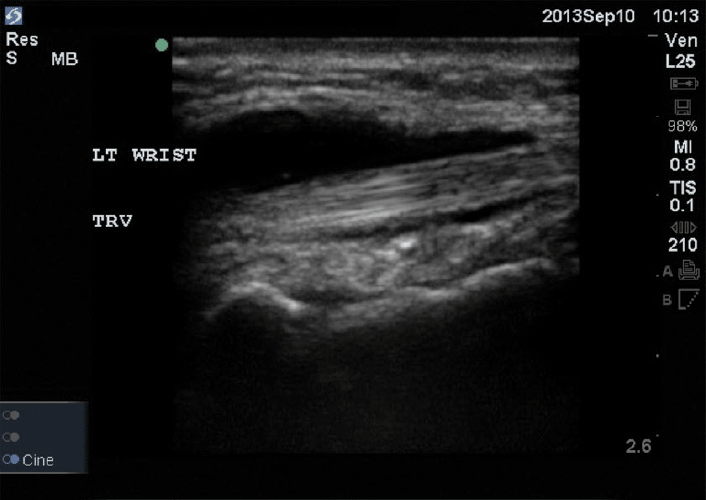
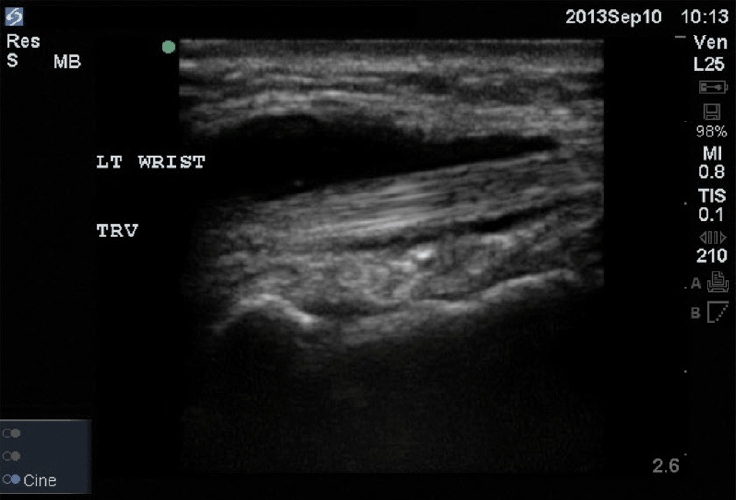
Exam shows dorsal erythema over the wrist with pain with both active and passive flexion and extension of the wrist. No deformities, loss of nerve function, or limitations of movement. A bedside ultrasound is performed to aid diagnosis.
Case 2. The Patient
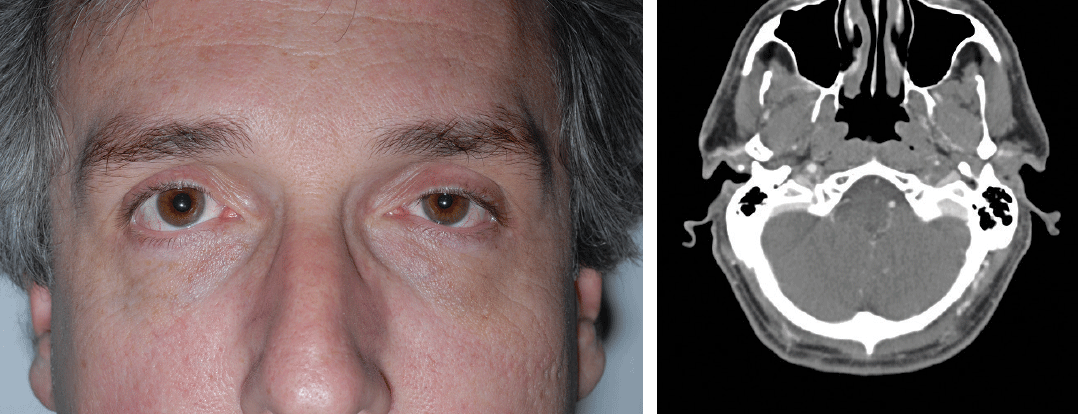
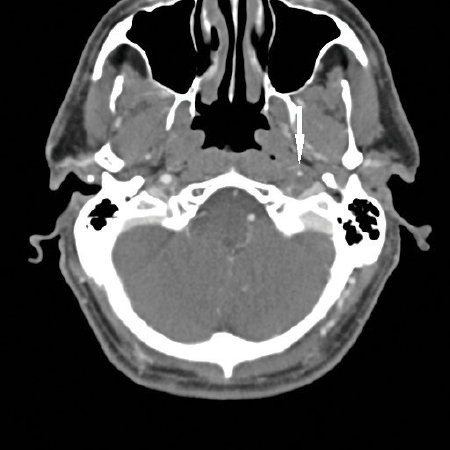
A 42-year-old male presents to an urban tertiary care ED with a two-week history of left eyelid droop and headache. His headache is primarily left-sided, and he noticed the eyelid droop two days after the onset of his headache. He originally presented to an outside ED and underwent a negative non-contrasted CT of the head. He was then referred to a neurologist and had a normal outpatient MRI/MRA of the brain. As his symptoms persisted, he decided to seek emergent care. On presentation his examination is remarkable only for the findings seen in the images provided. Due to his history and findings, a CT angiogram of the neck was performed, with findings as shown.
[hr gap="0"]
Case 1. The Diagnosis
This patient has infectious extensor tenosynovitis. This is an infection of the extensor tendons of the wrist and hand, typically caused by Staphylococcus or Streptococcus species.1 The tendon runs through a synovial sheath, which allows it to glide through its range of motion. With inflammation of this synovial sheath, the patient experiences difficulty or pain with extension of the digit. Infection in this sheath can be potentially devastating, as it can cause permanent loss of function of the digit.3 A physical exam is sometimes enough to make the diagnosis, but in cases where there is some ambiguity, bedside ultrasound can be used as an adjunct.
Elevated pressure within the tendon shealth can affect the circulation to the tendon, causing necrosis.2 All patients with infectious tenosynovitis should be admitted and given intravenous antibiotics. A consult to hand surgery is always warranted, since most will require surgical incision and drainage.1 The patient in this scenario was started on double coverage IV vancomycin and clindamycin, and taken for operative drainage. He was found to have suppurative tenosynovitis of multiple extensor tendons. Intraoperative cultures later grew out Serratia and Staph. He was able to make a nearly complete recovery with only minimal loss of thumb extension.
Case 2. The Diagnosis
Horner's syndrome secondary to left internal carotid artery (ICA) dissection. A painful headache with Horner's syndrome is present in 44% of extracranial ICA dissections.1,2
Interestingly, along with the left ptosis and miosis seen in the images, the patient complained of left forehead anhidrosis, demonstrating a full Horner's syndrome. CT angiography confirmed his ICA dissection as the etiology of his symptoms (note the markedly narrowed lumen of the left ICA as opposed to the right). Other causes of Horner's syndrome include strokes, cervical trauma, cavernous sinus pathology, malignancies, or any other interruption of a three-neuron sympathetic pathway.3 Workup in the ED involves imaging targeted toward suspected underlying etiologies, typically involving neurovascular imaging of the head and neck. In children, the presence of acute Horner's syndrome should prompt evaluation for tumor, especially paraspinal neuroblastoma.4-5
IMAGES PROVIDED BY R. JASON THURMAN, MD
REFERENCES
- Kanavel AB: Infections of the Hand. 6th ed. Philadelphia, Lea & Febiger, 1993.
- Lyn E, Maihot T: Rosen's Emergency Medicine Concepts and Clinical Practice, 8th ed. Elsevier Health Sciences, 2014.
- Small Ln, Ross JJ: Suppurative Tenosynovitis And Septic Bursitis. Infect Dis Clin North Am 2005; 19:991.