Ultrasound-guided subclavian vein access is a safe, effective and efficient option for central venous cannulation. Using ultrasound can decrease the time to cannulation in addition to many of the feared complications.
Case
A 75-year-old morbidly obese female with a history of diabetes, CHF, and CAD presents to your ED in septic shock secondary to C. diff. colitis. Her blood pressure does not respond to her initial 30 cc/kg bolus, and you decide it’s time for central line placement and vasopressors. With her large pannus and c diff. infection, femoral cannulation is undesirable, and when you attempt to lay her down in Trendelenburg (or even flat), she becomes severely dyspneic.
Questions
- What are your next steps?
- If you choose subclavian access, what are the benefits? What are the potential complications?
- How can your optimize your chance of success and minimize the risks?
You decide the subclavian vein is your best access option. There are potential hazards, but you realize you can reduce the likelihood of these and increase your chance of success by using ultrasound.
Anatomy 3
The subclavian vein is the continuation of the axillary vein as it courses beneath the clavicle. It travels superiorly starting at the lateral border of the first rib, then under the clavicle medially until it joins the internal jugular vein. The subclavian artery runs superior and posterior to the subclavian vein. Importantly, the lung and pleural cavity lie deep and inferior to the subclavian vein and are particularly vulnerable to accidental puncture on the left chest (as compared to the right) where the apex of the lung can extend above the first rib. The brachial plexus courses superiorly and deep to the medial portion of the subclavian artery, and the thoracic duct lies on the left side.
Figure 1. Subclavian Anatomy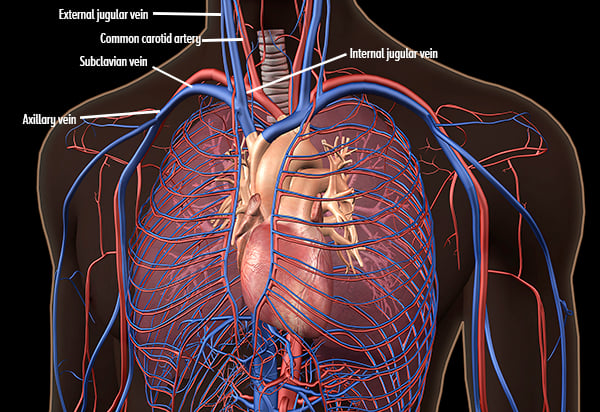
Technique
Utilizing the high-frequency linear probe, the subclavian vein can be approached in either the short or longitudinal axis.
|
|
Short-axis |
Longitudinal-axis |
|
Ultrasound View |
SCV: Subclavian vein; SCA: Subclavian artery
|
a. Cephalic vein; b. Axillary vein; SCV: Subclavian vein
|
|
How-to |
Place the long footprint of the US probe perpendicular to the course of the vessel with the indicator pointed toward the patient’s right |
Place the long footprint of the US probe parallel to the course of the vessel (or find the short axis and rotate 90 degrees) |
|
Pros |
Typical approach for US-guided lines (muscle memory) |
In-pane so you can visualize the needle tip and shaft during catheterization |
|
Cons |
Out-of-plane so visualizing the needle tip can be challenging |
Cannot visualize both artery and vein simultaneously, requiring the operator to confirm vessel prior to cannulation |
Anatomically, the subclavian vein can be accessed utilizing a supraclavicular or infraclavicular approach.
Supraclavicular Approach
To cannulate the vein in the supraclavicular approach, stand at the head of the bed as if placing an internal jugular line. Place the probe above the clavicle and visualize the vein. You may want to find the internal jugular vein first and trace it distally until it joins the subclavian. Position your needle tip at the center of the probe and puncture the skin, traversing the fascial planes. Continue to visualize the needle tip until it enters the vessel. Insert the guidewire once the needle is in the lumen of the vessel. Withdraw the needle, continue with scalpel incision and dilatation, and insert the catheter over the guidewire. Of note, you will always utilize the short axis view when employing the supraclavicular approach.
Figure 2: Subclavian vein (SCV)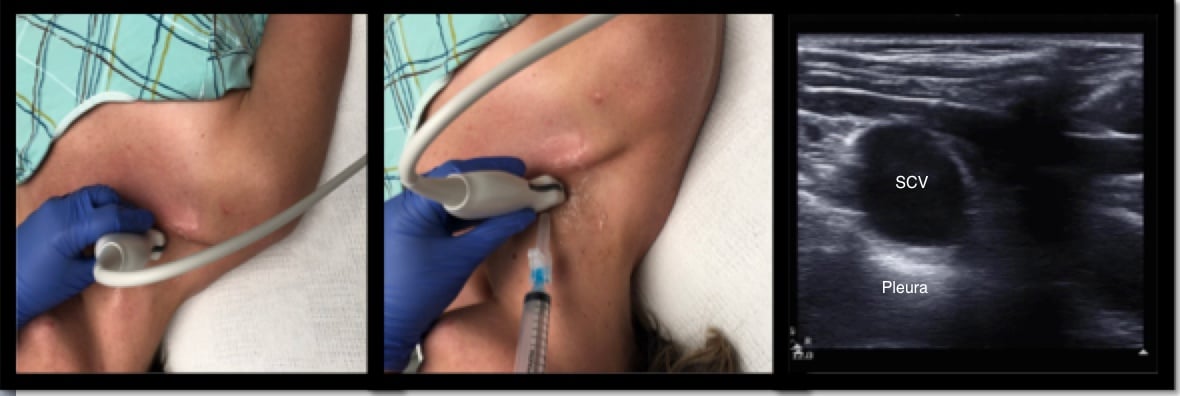
Infraclavicular Approach
With the patient in the supine position (if possible), place the probe in the infraclavicular fossa and identify the vasculature 2-3 cm distal to where the subclavian vein courses below the clavicle. Cannulation occurs more laterally as compared to the landmark approach. Obtain a long-axis view of the axillary vein and distal subclavian vein. Use compressibility and/or pulse-wave Doppler to confirm visualization of the vein (as opposed to the artery). Take note of the lung pleura beneath the vessels. Insert the needle at the midpoint of the short footprint of the probe and continue to visualize the needle in long axis as it approaches the vessel. Once the needle is visualized in the lumen, insert the guidewire, monitoring placement dynamically with ultrasound. After scalpel incision and dilatation, insert the catheter over the guidewire.
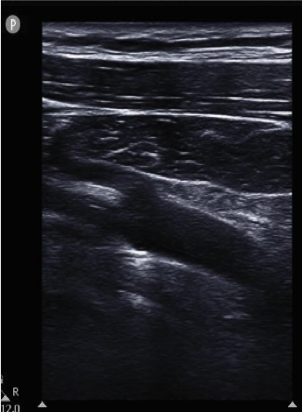
Figure 3: a. Cephalic vein; b. Axillary vein; SCV: Subclavian vein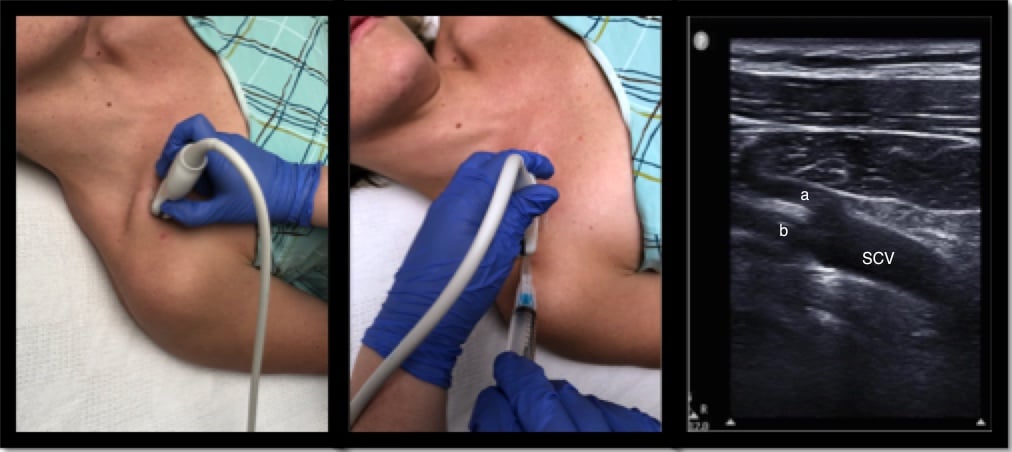
Another option is to approach the subclavian vein infraclavicularly in the short axis, as seen below. Note the difference in probe position for obtaining a short axis versus long axis view is quite minimal, requiring only small movements to obtain.
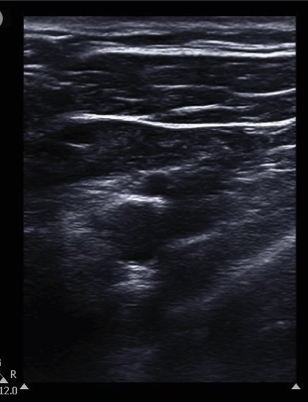
Figure 4: SCV: Subclavian vein; SCA: Subclavian artery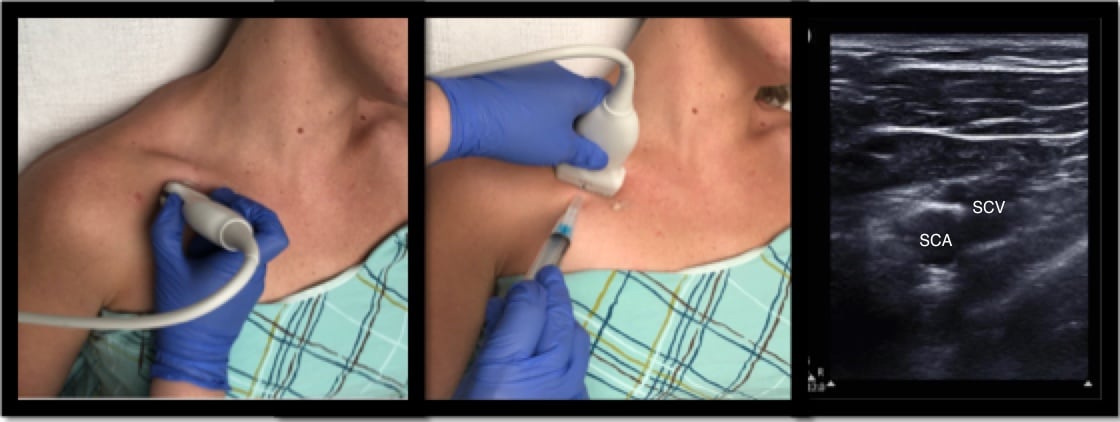
Questions Revisited
- What are your next steps?
- If you choose subclavian access, what are the potential benefits? What are the potential complications?
- How can your optimize your chance of success and minimize the risks?
Using the high-frequency probe in a longitudinal, infraclavicular approach, you cannulate the subclavian vein on the first try. You confirm placement and your patient receives the care she needs.
There are a multitude of benefits to subclavian vein access. Subclavian lines have been associated with fewer cases of thrombosis and infection (though recent studies show less significant differences in infection rates between femoral, internal jugular, and subclavian vein access due to sterile practices).1,5,6 The subclavian vein often remains patent in hypovolemic patients and is frequently more accessible in the setting of cervical spine or pelvic trauma or when the patient is unable to tolerate a Trendelenburg position. Potential complications include the risk of arterial cannulation (and decreased ability to apply pressure secondary to the anatomical location relative to the clavicle), pneumothorax, nerve injury, hematoma, hemothorax, or thoracic duct injury. Some studies list complication rates with blind technique as high as 18.8%.5
Ultrasound helps improve upon these benefits and mitigate such risks. Studies have revealed increased cannulation success with fewer attempts and decreased time to successful cannulation with the use of ultrasound. Furthermore, ultrasound use is associated with a decreased rate of pneumothorax, hematoma, and arterial puncture. Some providers have limited experience with this technique, which can pose a challenge. Additionally, there is limited data regarding ultrasound-guided subclavian approach. Practice is integral to gain the full benefits of ultrasound-guided subclavian access.
Bottom Line
Ultrasound-guided subclavian vein access is a safe, effective and efficient option for central venous cannulation. Using ultrasound can decrease the time to cannulation in addition to many of the feared complications. However, more data and practice with the technique may be required for providers to feel comfortable with this under-utilized access option.
References
1. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. How do ultrasound guidance and anatomical landmarks compare for subclavian or femoral vein catheterization? Cochrane Database Syst Rev. 2015;1:CD011447.
2. Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study. Crit Care Med. 2011;39(7):1607-1612.
3. Heffner A, Androes M. Placement of subclavian venous catheters. UpToDate. Topic 15673 Version 12.0.
4. Marik PE, Flemmer M, Harrison W. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: A systematic review of the literature and meta-analysis. Crit Care Med. 2012;40(8):2479-2485.
5. Merrer J, De Jonghe B, Golliot F, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: A randomized controlled trial. JAMA. 2001;286(6):700-707.
6. Miller AH, Roth BA, Mills TJ, Woody JR, Longmoor CE, Foster B. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the Emergency Department. Acad Emerg Med. 2002;9(8):800-805.
7. Rezayat T, Stowell JR, Kendall JL, Turner E, Fox JC, Barjaktarevic I. Ultrasound-guided cannulation: Time to bring subclavian lines back. West J Emerg Med. 2016;17(2):216-221.
8. Vogel JA, Haukoos JS, Erickson CL, et al. Is long-axis view superior to short-axis view in ultrasound-guided central venous catheterization? Crit Care Med. 2015;43(4):832-839.