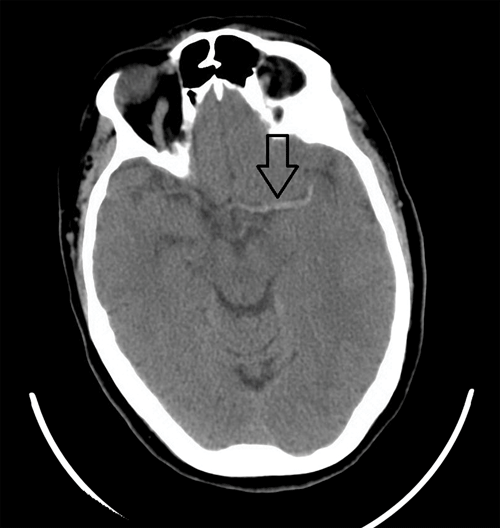
A 60-year-old female presents to the ED with altered speech and decreased responsiveness that began less than one hour ago. Outside of a resolving hypoxia, all vital signs are stable. She has a noticeable right-sided facial droop, is non-verbal, is unable to follow commands but withdraws from pain, and has an up-going Babinski reflex on the right. A stroke alert is called and a non-contrast computed tomography scan (CT) of her head is obtained. This reveals a dense middle cerebral artery (MCA) sign on the left without any sign of hemorrhage as seen in Image 1. The patient is treated with IV tPA and transferred to a tertiary care center where she undergoes computed tomography angiography (CTA) and CT perfusion scans, followed by endovascular thrombectomy. She is continued on anticoagulation and undergoes rehabilitation, after which her only residual symptom is a slight delay in her right hand when playing the piano.
Acute ischemic stroke is a common life threatening condition seen in the ED every day. In the United States, approximately 795,000 people experience a stroke annually; 87% of these are ischemic.1 After the physical exam, the standard of care is that a non-contrast CT be the next step in diagnosis of a potential stroke. Although its greatest value is in ruling out a hemorrhagic stroke, emergency physicians should be familiar with findings on non-con CT that provide evidence for an ischemic stroke. Additionally, we are on the prepuce of an era in which endovascular therapies could potentially replace current treatment algorithms. In these new testing protocols CTA and CT perfusion scans, in addition to the non-con CT, are the tests of choice for selecting patients that would benefit from interventional therapies.
Discussion
The ability to interpret non-contrast head CTs in the evaluation of stroke is a necessary skill for all emergency providers. It is an essential test for all potential stroke patients when intervention is time sensitive and can determine patient outcome. Obtaining a non-contrast head CT for all potential stroke patients as early as possible determines our management and is the most cost-effective imaging strategy to improve their survival and quality of life.2 An emergency physician should not limit their reading of a non contrast head CT to only evaluating for presence or absence of hemorrhage. There are several early signs of ischemic stroke that are often present, as seen in Table 1.3,4
The hyperdense MCA sign in particular is a marker of a thromboembolic occlusion of the M1 segment of the MCA. This sign is usually associated with large territory infarcts and is present in 17-50% of MCA strokes.5 One prospective study of 443 patients with cerebral vascular accidents found the hyperdense MCA sign to be only 30% sensitive, but 100% specific for large territory infarction.6 Despite its strong association with large territory infarcts, its association with poor outcome is controversial. Part of this ambiguity may be explained by the pseudohyperdense MCA sign, or mimickers of the hyperdense MCA sign. The pseudohyperdense MCA sign looks similar to the hyperdense MCA sign, but it is caused by an unrelated mechanism such as intravenous contrast medium, vascular calcification, or an elevated hematocrit. The two signs can be distinguished by measuring the attenuation of the sign compared to the same artery segment on the contralateral side, or by observing resolution of the sign on repeat CT (depending on the cause for the finding).5,7
A systematic review of 15 studies and 3,468 patients found the prevalence of the signs in Table 1 to be only about 61% (+/-21%), with a mean sensitivity of 66% (range of 20-87%), and mean specificity of 87% (range of 56-100%).3 In this study, the presence of one of these signs elevated the risk of a poor outcome (odds ratio of 3.11); however, there was no association in outcome when IV thrombolysis was given to a patient in whom a sign was present.4 Another study found a similar lack of association between outcome and the presence of these signs in patients receiving IV alteplase (tPA).8 Therefore, despite these signs being associated with poor outcomes, in our current treatment algorithm of IV tPA vs no IV tPA, early CT signs of acute ischemic stroke should not play a significant role in decision making and management.
The utility of the hyperdense MCA sign is found when it is used as a representative of a proximal thromboembolic occlusion of the MCA.5 This finding then justifies further studies. Endovascular clot retrieval therapy may play a role; in select patients it has been shown to improve functional outcomes compared to standard therapy with or without IV tPA. Three recent randomized controlled studies (EXTEND-IA, ESCAPE, and SWIFT PRIME trials) demonstrated a benefit to clot retrieval in selected patients.9,10,11 These trials utilized either CTA or CT perfusion scans to select patients with relatively small irreversible infarct territories and a proximal occlusion of the internal carotid or an intracerebral artery (i.e., the MCA). The ESCAPE trial included patients up to 12 hours after symptom onset, providing endovascular clot retrieval long after IV tPA becomes contraindicated (at 3 or 4.5 hours, depending on the patient and existing protocols).10 A hyperdense MCA sign on the non-contrast CT may prompt the emergency provider to consult a stroke specialist and obtain one of these additional scans or further intervention.
Table 1. Early Signs of Ischemic Stroke on Non-Contrast CT3,4
Hyperattenuation of a large vessel (ex. hyperdense MCA sign)
Hypoattenuation of 1/3 or more of the MCA territory
Loss of the insular ribbon
Loss of gray-white matter differentiation
Cortical sulcal effacement
Focal parenchymal hypoattenuation
Obscuration of the lentiform nucleus
Alberta Stroke Programme Early CT Score (ASPECTS)
Conclusion
At this point, there is no evidence that associates the hyperdense MCA sign or any early sign of ischemic stroke on non-contrast CT with endovascular therapies and improved outcomes. But, as more literature is published on these new therapies, it may be even more important for the emergency provider to correctly identify proximal cerebral artery strokes to hasten endovascular intervention.
References
- Mozaffarian D, Benjamin EJ, Go AS, et al: Heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation 131(4):e29-e322, 2015.
- Wardlaw JM, Seymour J, Cairns J, et al: Immediate computed tomography scanning of acute stroke is cost-effective and improves quality of life. Stroke 35(11):2477, 2004.
- Wardlaw JM, Mielke O: Early signs of brain infarction at CT: observer reliability and outcome after thrombolytic treatment--systematic review. Radiology 235(2):444, 2005.
- Rdhiana H, Syazarina SO, Shahizon Azura MM, et al: Non-contrast Computed Tomography in Acute Ischemic Stroke: A Pictoral Review. Med J Malaysia 68(1):93-100, 2013.
- Shetty SK: The MCA Dot Sign. Radiology 241(1):315-8, 2006.
- Leys D, Pruvo JP, Godefroy O, et al: Prevalence and Significance of Hyperdense Middle Cerebral Artery in Acute Stroke. Stroke 23:317-324, 1992.
- Jha B, Kothari M: Pearls & Oysters: Hyperdense or pseudohyperdense MCA sign: A Damocles sword? Neurology 72:e116-e117, 2009.
- Patel SC, Levine SR, Tilley BC, et al: Lack of clinical significance of early ischemic changes on computed tomography in acute stroke. JAMA 286(22):2830, 2001.
- Campbell BCV, Mitchell PJ, Kleinig TJ, et al: Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection. N Engl J Med 372:1009-1018, 2015.
- Goyal M, Demchuk AM, Menon BK, et al: Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N Engl J Med 372:1019-1030, 2015.
- Saver J, Goyal M, Bonafe A, et al: Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N Engl J Med 2015 Apr 17. [Epub ahead of print] DOI: .1056/NEJMoa1415061. https://urldefense.proofpoint.com/v2/url?u=http-3A www.nejm.org_doi_pdf_10.1056_NEJMoa1415061&d=AwIFaQ&c=4R1YgkJNMyVWjMjneTwN5tJRn8m8VqTSNCjYLg1wNX4&r=iHJZMnLgRTPtJLiKLIB9MM-ZkgILN8M_fDYZCRbDkes&m=AXeHw5umDXE1v2EKiMyj8u09w10ZjACYvdoeCWWQlaQ&s=Y_EHR2u9V5EYA-GmRpMftwR9X2-JcElYiw2z1necsIk&e=