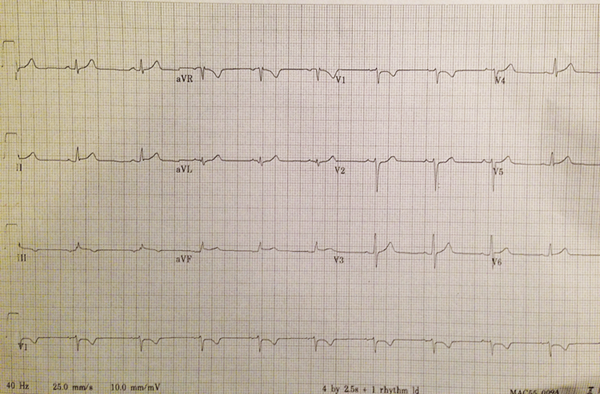
A 26-year-old anxious, diaphoretic male presents with crushing mid-sternal chest pain that awakened him from sleep. Past medical history is unremarkable aside from an upper respiratory infection 1 week ago. He has a family history of coronary artery disease. His vital signs are within normal limits, and he has a normal cardiopulmonary exam. His ECG is shown (Figure 1).
Cardiology is consulted because of concern for ST-segment elevation inferiorly, and the cath lab is activated. Workup reveals troponin of 0.34 ng/mL. The catheterization is clean, and the patient is diagnosed with perimyocarditis.
Pericarditis is defined as inflammation of the pericardium, which consists of the visceral pericardium overlying the epicardium and the parietal pericardium surrounding the heart. The space between these two layers is the pericardial cavity, which normally contains up to 50cc of fluid. Pericarditis is the most common disorder involving the pericardium.
Myocarditis, or inflammatory cardiomyopathy, is inflammation of the heart muscle itself and is a separate disease entity, even though it may be accompanied by pericarditis. Both myocarditis and pericarditis are most commonly diagnosed in the setting of a recent viral infection, although in several studies, an etiology was identified in only 17% of cases.1,2,3
Diagnosis
The major clinical manifestations of pericarditis include sharp or pleuritic chest pain that is often relieved by sitting up, a pericardial friction rub, suggestive ECG changes, and a pericardial effusion.4 The transient friction rub is best heard at the left lower sternal border and has been reported in up to 35% of cases.5,6 Another study reported the presence of a pericardial effusion in 60% of patients, with signs of cardiac tamponade in 15% of patients presenting with pericarditis.4
Laboratory findings include elevated CRP, ESR, and WBC. If myocarditis is present in conjunction with pericarditis, then cardiac biomarkers may also be elevated. In one study, Troponin I was elevated in 34% of patients, whereas CK-MB was elevated in only 5.7% of patients.7 Another study found that Troponin T was elevated in 93% of patients with immunohistologically proven myocarditis.8
ECG Findings
The electrocardiogram is the most important tool for diagnosing pericarditis. The provider must be certain that the patient is not having an ST-segment myocardial infarction (STEMI).
Classic ECG findings in pericarditis include widespread PR-segment depression and concave ST-elevations (STE) with reciprocal changes in leads aVR and V1. In general, there are 4 steps to differentiate between pericarditis and STEMI. If the answer is “YES” to question 1, 2, or 3, then the diagnosis is STEMI. If the answer is “NO” to questions 1-3, then move to question 4, which points to pericarditis.
1) Are there ANY ST depressions other than in leads aVR or V1?
2) Are there ANY convex up or horizontal STEs?
3) Is the STE greater in lead III than lead II?
4) Look for PR depression in multiple leads
A useful finding reported in up to 80% of cases with pericarditis is Spodick's sign, a down-sloping of the TP-segment that is best visualized in the lateral precordial leads, as well as in lead II.8,9
Treatment and Disposition
Pericarditis usually follows a benign course lasting 1-2 weeks and can be treated in the outpatient setting with high dose aspirin or NSAIDs. Specific clinical features such as fever >38 degrees Celsius, subacute course, large effusion or tamponade, immunosuppression, and aspirin or NSAID failure may be indicators of poorer prognosis or increased risk of complications.4 These patients should be hospitalized.
Case Conclusion
This patient's ECG does not fit perfectly into either the “STEMI” or “pericarditis” box. The only ST-segment depression is in lead V1. There are no convex STEs, but there are subtle horizontal STEs in leads II, III, and aVF. The STE is not greater in lead III than in lead II. Lastly, there is PR-segment depression in leads II and aVF.
The patient was admitted to a telemetry floor and had an uneventful hospital stay. His original ECG changes returned to normal by day 4, and he was subsequently discharged with close follow-up.
References
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75(5):378.
- Permanyer-Miralda G, Sagristá-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patient. Am J Cardiol. 1985;56(10):623.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115(21):2739.
- LeWinter MM. Acute Pericarditis. N Engl J Med. 2014;371:2410-2416.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43(6):1042.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75(5):378.
- Smith SC, Ladenson JH, Mason JW, Jaffe AS. Elevations of cardiac troponin I associated with myocarditis. Experimental and clinical correlates. Circulation. 1997;95(1):16.
- Spodick DH. Electrocardiogram in acute pericarditis. Distributions of morphologic and axial changes by stages. Am J Cardiol. 1974;33(4):4704.
- Ginzton LE Laks MM. The differential diagnosis of acute pericarditis from the normal variant: new electrocardiographic criteria. Circulation. 1982;65:1004-1009.