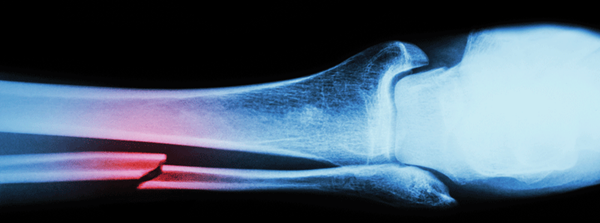
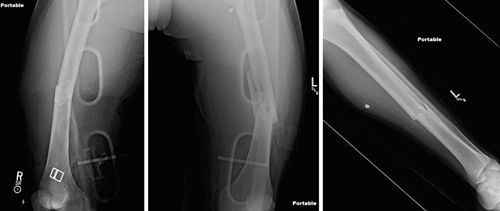
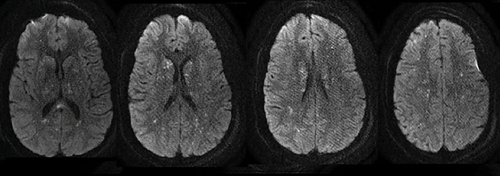
EMS brings in a 20-year-old male who jumped from an overpass in a suicide attempt. He arrives with normal hemodynamics and is found to have bilateral mid-shaft femur and left tibial shaft fractures (Figure 1). Further workup reveals no other injuries. He is placed in traction, splinted, and admitted to orthopedics. While awaiting an inpatient bed in the emergency department, he has sudden onset tachycardia to the 140s, hypoxemia to 80s on room air, and a decreased level of consciousness. Intubation improves his hypoxia, but he remains obtunded with extensor posturing and a fixed rightward gaze. Chest computerized tomography (CT) shows bilateral diffuse interlobular septal thickening and ground-glass opacities. Head CT reveals no pathology. Magnestic resonance imaging (MRI) of his brain reveals a “star-field” pattern of innumerable, diffuse, punctate lesions concerning for cerebral fat emboli syndrome (Figure 2).
Background
Fat embolism refers to the presence of fat globules in the pulmonary microcirculation, and it usually occurs after a long bone fracture or other major trauma. Although fat emboli can be detected in the lungs of as many as 90% of individuals with long-bone fractures, they are rarely clinically significant. Fat embolism syndrome (FES), on the other hand, is a systemic inflammatory cascade and serious consequence of fat emboli described as a certain pattern of clinical signs and symptoms. FES can occur from 30 minutes to 48 hours after injury, and is seen in up to 3% of patients with a single long bone fracture with reports as high as 33% in patients with bilateral femur fractures.2 The risk is thought to be reduced by early immobilization and early operative correction.
Unfortunately, there is no gold standard test for the diagnosis of FES. However, several clinical criteria have been proposed. The most commonly used are Gurd's Criteria (Table 1).3 These clinical criteria are based on the presence of respiratory symptoms, neurologic abnormalities, and a petechial rash. Radiologic findings are helpful but not diagnostic for FES. Chest imaging may show nonspecific bilateral patchy opacities. Head CT may be normal, and MRI brain may show a “star-field” pattern of diffuse, punctate, hyperintense lesions on diffusion-weighted imaging. Fundoscopy may demonstrate cotton wool spots, hemorrhages, and retinal edema.3
Pathophysiology
The pathophysiology of FES is poorly understood. Intravascular embolization of fat globules into damaged venous sinuses likely triggers the syndrome. These emboli then gain access to the arterial system, as their small size allows a percentage to pass through the pulmonary capillaries. The fat emboli then cause both pulmonary and cerebral vasculature occlusion and local inflammation. Another theory suggests that fat emboli precipitate intravascular lipolysis, releasing toxic free fatty acids systemically. This generates a local and systemic inflammatory reaction leading to cerebral vascular injury, with neurologic effects related to infiltration of inflammatory cells instead of mechanical occlusion.3,4
Management
The management of FES is supportive. Other treatable causes of neurological decline such as intracranial hemorrhage, diffuse edema, contusions, or herniation should be ruled out. Once diagnosed, the cornerstone of treatment is treating hypovolemia and hypoxia, and operative stabilization of fractures. Patients usually require ICU management for close neurologic monitoring and supplemental oxygen or ventilatory support. Cerebral edema often ensues, and case reports have described midline shift requiring neurosurgical decompression; thus, any change in mental status, hemodynamic instability, or sign of impending herniation should prompt a stat head CT and neurosurgical consultation with early consideration for intracranial pressure monitoring.4 Some small randomized controlled trials have suggested the use of steroids to both prevent and treat FES, but there have been no large conclusive studies.4
Prognosis
An overall mortality of 5-15% has been described.5 In a review of literature from 1980 to 2012, fifty four cases of FES with cerebral involvement were identified.6 Of these patients, good neurologic outcome (intact or mildly disabled) was seen in 58% of patients with coma and/or abnormal posturing on presentation, and in 91% of patients with mild mental status changes, focal deficits, or seizure on presentation. While neurologic recovery can be delayed by weeks to months, because the pathophysiology is thought to include inflammation rather than neuronal death, a higher chance of recovery has been seen than in comparable ischemic lesions.
Case Conclusion
The patient was admitted to the ICU. Echocardiogram demonstrated a patent foramen ovale, likely contributing to his significant burden of disease. Over time his neurologic exam improved, with resolution of posturing and increasing spontaneous movement. He was eventually extubated. Approximately one month after the onset of his FES, he was discharged to a rehabilitation facility with residual mild strength deficits in his left upper and lower extremities. He was alert and oriented with daily improvement of his cognitive communication impairments.
Table 1. Gurd's Diagnostic Criteria for Fat Embolism Syndrome*
| Major Criteria | Minor Criteria |
|
|
*Diagnosis requires one major and 4 minor criteria.
**Radiographic changes classically include focal areas of ground glass opacification with interlobular septal thickening, but can occasionally include nodules and vascular filling defects.
References
- Bulger EM, Smith DG, Maier RV, Jurkovich GJ. Fat embolism syndrome. A 10-year review. Arch Surg. 1997;132:435-439.
- Johnson MJ, Lucas GL. Fat embolism syndrome. Orthopedics. 1996;19:41.
- Kosova E, Bergmark B, Piazza G. Fat embolism syndrome. Circulation. 2015;131(3):317-20.
- Sen RK, Tripathy SK, Krishnan V. Role of corticosteroid as a prophylactic measure in fat embolism syndrome: a literature review. Musculoskelet Surg. 2012;96:1-8.
- Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56:145-54.
- Kellogg RG, Fontes RBV, Lopes DK. Massive cerebral involvement in fat embolism syndrome and intracranial pressure management. J Neurosurg.2013;119(5):1263-70.