Introduction
More than 2.5 million eye injuries occur each year.1 According to information gleaned from the Healthcare Cost and Utilization Project (HCUP), there were 636,619 emergency department visits related to eye injuries in 2008, representing an average of 1,744 ED visits daily.2 Blunt orbital trauma is a significant cause of ocular morbidity and among the common preventable causes of monocular blindness in developed countries, and is encountered in the ED on a regular basis.3,4,5 An efficient, organized approach to the assessment of blunt orbital trauma in the ED is essential.
Epidemiology
The statistical brief compiled from the HCUP reports that men sustained eye injuries more commonly than women. This was specifically true in men younger than 44 years old.2 The most common eye injury seen in the ED was to the superficial cornea. The most common cause of eye injury seen in all 2008 ED visits was the result of the eye being struck by, or against, an object. This was followed by falls and then burns as the second and third most common causes of injury. Patient injuries requiring admission to the hospital were most commonly the result of falls, motor vehicle accidents, or the eye being struck by or against an object, in that order.2 Recently, Cheung, et al, analyzed injury data and noted that a conservative lifetime prevalence of eye injury in the general population is 14.4%.4 This study found the most common cause of hospital-based ocular emergencies was motor vehicle accidents followed by falls.4 They found that in their study population the most common diagnoses were ocular contusions with underlying orbital fractures, orbital trauma, and posterior segment disease.4
Emergency department evaluation of blunt orbital trauma
Emergency department evaluation of any orbital trauma should begin with the history. The patient should be queried about the nature of the injury, the mechanism, and the circumstances under which the injury occurred. The timing of the injury is also important and may change the management and disposition. The patient should be asked about visual changes following the event, his or her pain level, and if there are any entoptic phenomena (new onset of flashing lights, floating spots, or positive scotomata). The physician should gather history of previous eye injury or eye disease. Additional pertinent history includes the use of contact lenses or spectacles, any history of previous ocular surgeries, any regular use of ocular medications, a general health history, and a history of known allergies.
A general impression or external inspection can be made during the interview. Make note of adnexal lacerations, incisions, eyelid ecchymosis, eyelid abnormalities, globe displacement, extraocular muscle motility limitations, subconjunctival hemorrhage, conjunctival injection, or corneal abrasions.
The sequelae of blunt orbital trauma fall over a broad spectrum from simple, isolated soft tissue contusions to frank globe rupture. Adjuncts such as radiographic imaging should be used where applicable to facilitate diagnosis and timely, appropriate ophthalmologic disposition.
Be prepared
You will need some basic tools to effectively evaluate the injured eye in the emergency department (Table 1).
Table 1. Basic Tools for ED Eye Exam
- Snellen eye chart or pocket
- Transilluminator (penlight)
- Handheld Wood's lamp
- Slit lamp
- Handheld, direct ophthalmoscope
- Tonometer
- Fluorescein dye, anesthetic drops (alcaine, tetrcaine)
- Metal or plastic eye shield
- Tape
Visual acuity
Visual acuity should be tested in every patient who presents with any eye complaint. This is the eye's vital sign. Acuity should be documented just after the history (Table 2). If the patient cannot open their eyes because of photophobia, blepharospasm, or lid edema, the acuity must still be attempted, but if unable to be adequately assessed, it should be documented as such. In these cases, instillation of a topical anesthetic to allow for improved patient comfort can sometimes facilitate the exam.6
External inspection: Soft tissues, facial bones, orbital rim
External inspection should include the periorbital soft tissues, the lids, and the orbital bones, noting any lacerations, abrasions, contusions, or edema. All involved areas should be palpated for subcutaneous emphysema or crepitance.7 The facial and orbital bones should also be palpated to determine extension of injury. The presence of epistaxis may suggest a medial wall intrusion.7 Orbital wall fractures have the capability of inducing bleeding and subsequent proptosis secondary to increased orbital fluid volume. The globe may be proptotic secondary to orbital fat herniation, or it may be enophthalmic secondary to extraocular muscle entrapment. This may or may not be obvious on external exam.
In any ocular trauma, it is important to evaluate the nerves of the face for sensory deficits, specifically in the V2 distribution (the maxillary nerve).7 This nerve is in a particularly vulnerable position as it exits from the infraorbital rim. Often, the increased intraorbital pressure in trauma, in concert with a weak orbital floor, allows for herniation of the orbital soft tissues into the maxillary sinus below. A study by Kreidl, et al, investigated the significance of intraocular sequelae following blunt orbital trauma. They found that there was a higher rate of significant intraocular sequelae in patients who did not sustain orbital fractures, suggesting that the orbital floor, or “blow out,” fracture may in fact be protective for the globe.3,8 Previous studies did not share this data and conclusion, however.3
Many times, the lid and periorbital soft tissue edema is so severe that the lids cannot be easily or adequately retracted, making assessment of the globe and surrounding structures difficult (Image 1). A Desmarres lid retractor (Image 2) or a retractor improvised from a paper clip can be used to raise the superior lid.6 Ocular ultrasound (US) may be useful in this setting and may be a more comfortable approach to evaluating structures behind the edematous lids.9 Excess pressure on the globe should be avoided during the exam.
The use of the swinging flashlight test to assess the visual system for a relative afferent pupillary defect (RAPD, or Marcus Gunn pupil) is important early in the examination process.6 This test compares one eye's afferent prechiasmal pathway to the efferent pathway of the other eye. When a light is shined into one eye, constriction is expected in the contralateral pupil. This serves primarily as a stimulus-protective response. It occurs via the consensual reflex nerve pathway which connects via the Edinger-Westphal nucleus in the midbrain. When the flashlight is swung between the two eyes, the direct response of each eye can be seen. Contralateral pupillary dilation indicates that the pathway on that side is sending less stimulation into the system than the eye where the flashlight just was. This objective test cannot be manipulated by the patient and demonstrates the existence of true ocular pathology.
Cornea and conjunctiva
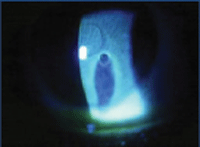
The emergency physician can begin ocular structure assessment with gross inspection of the conjunctivae. Complete inspection includes eversion of the superior lid. Any superficial foreign bodies, including contact lenses, should be removed. The slit lamp with a cobalt blue filter or Wood's lamp can be used in combination with fluorescein dye to evaluate the cornea and conjunctiva for defects. If there is suspicion for corneal perforation, the Seidel test should be performed. This is done by painting the lesion with fluorescein dye. If the dye is displaced inferiorly by fluid moving away from the lesion, the test is positive for perforation (Image 3).
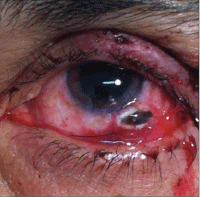
Subconjunctival hemorrhage (SCH) serves as a clue to the extent of trauma. The larger and more extensive the subconjunctival bleeding, the more extensive and severe the injury is likely to be.10 In instances of large SCH, where visual inspection is inhibited, more advanced imaging may be indicated to rule out globe rupture. The weakest portions of the globe are under the bellies of the recti muscles, at the limbus, and around the posterior scleral foramen.10
Anterior chamber, iris, and pupil
A slit lamp should be used when at all possible to evaluate the adnexa and anterior chamber. The evaluation should include examination for foreign material, lacerations, hyphema (blood in the anterior chamber), anterior chamber inflammation (cells and flare), iridodialysis (the “D”-shaped pupil), iris tears (polycoria, ectopic pupillae), penetrating iris injuries (the “peaked” pupil), abnormalities of the angle (cyclodialysis), dislocated lens (luxation), or a lens entrapped in the pupil.
Patients with hyphema may present with the classic signs of uveitis, including painful photophobia, conjunctival hyperemia, blurred vision, throbbing eye pain, lacrimation, and blepharospam.7 Intraocular pressure (IOP) should be assessed with a tonometer. Any time IOP is elevated following blunt traumatic ocular injury, a hyphema should be suspected, whether or not blood is visible in the anterior chamber. The colloquial term “eight-ball hemorrhage” connotes complete filling of the anterior chamber with blood and is so named because when an anterior chamber fills with clotted blood, it appears black, like a billiard ball. Complications of hyphema include corneal blood staining and hemolytic glaucoma secondary to angle blockage. While treatment is generally not complicated (cycloplegics, topical antibiotic and IOP control, and pain management), variations in anatomy and need for follow up usually warrants ophthalmology consultation.
Posterior chamber
Examining the posterior chamber with the slit lamp or the ophthalmoscope can be difficult in uncomplicated conditions, let alone following significant ocular injury with accompanying blepharospasm. If there is presence of a relative afferent papillary defect, poor visual acuity, or lack of red reflex, there should be concern for a complication in the posterior chamber. Given the time-sensitive nature and complexity of these injuries, ophthalmologic consultation is a must.
Globe rupture
Globe rupture, also termed scleral rupture, can occur via direct penetrating injury or as the result of blunt force trauma that elevates the intraocular pressure and exceeds the limits of the shell. Some globe ruptures are obvious, with extrusion of intraocular contents (lens, iris, or vitreous fluid), while others may be more subtle (Image 4). Indicators of potential globe rupture include subconjunctival hemorrhages expanding beyond 270 degrees around the limbus, an irregularly-shaped pupil, vitreous hemorrhage, and proptosis.6,10 When a ruptured globe is suspected, manipulation of the eye should be withheld to prevent accidental prolapse of additional tissue.6 This is an obvious ophthalmologic emergency, and the eye should be protected with a plastic or metal eye shield.6,7
Optic nerve injury
Traumatic optic neuropathy can occur directly or indirectly secondary to the closed compartment forces following injury-induced edema. Loss of vision, proptosis, visual field deficits, and relative afferent papillary defect are all suggestive signs.7
Retrobulbar hemorrhage
The bony orbit is composed of seven rigid bony walls (maxilla, frontal, zygomatic, ethmoid, sphenoid, lacrimal, and sphenopalentine). Anteriorly, the orbital septum and eyelids form another fairly inflexible boundary. The medial and lateral canthal tendons attach the eyelids to the orbital rim and limit the forward movement of the globe.11 Bleeding from injured orbital vessels into this volume-limited orbit has the potential to increase the volume, and thereby the intraorbital pressure. Pain, loss of vision (compressive optic neuropathy), and proptosis result as retro-orbital bleeding increases. This is termed orbital compartment syndrome, and it places the central retinal artery and vein at risk of collapse.6,11 It represents another absolute ophthalmologic emergency. Decompressive lateral canthotomy is the emergent treatment, and is within the scope of the ED physician, though it probably should be deferred to the ophthalmologist if they are readily available.6
Imaging
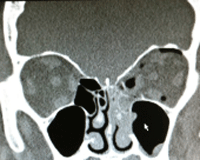
Maxillofacial CT scan, including the orbits, should be obtained for any presentation with significant mechanism of ocular injury (Image 5). In some busy emergency departments, there may be a delay in getting a CT scan due to department volume. Should this be the case, consider bedside ocular US. The use of the linear array probe to assess static orbital anatomy, as well as extra-ocular eye movements and pupillary reflexes, is described by Harries, et al.9 The literature also describes reviews of clinical cases in which the diagnosis of globe rupture, retrobulbar hematoma, lens dislocations, and retinal detachment were made through closed eyelids with use of the bedside US.12,13 Data continues to emerge for using bedside US as a determinate for intraocular pressure. Care should be taken not to exert undue pressure on the eye in case globe rupture is present.14 If your suspicion for rupture is high, US should probably be avoided.
Conclusion
Blunt ocular trauma presents a number of pathological entities that can have a profound and permanent effect on the patient's vision. Appropriate, logical, and systematic examination with proper first aid and timely consultation can reduce morbidity and provide for optimum recovery and outcomes.
REFERENCES
- American Academy of Ophthalmology. Eye Health Statistics at a Glance. Available at: http://www.aao.org/newsroom/upload/eye-health-statistics-april-2011.pdf. Accessed on February 10, 2014.
- Bureau of Labor Statistics. U.S. Department of Labor. The Editor's Desk. Workplace Injuries Involving the Eyes, 2008. Available at: http://www.bls.gov/opub/ted/2011/ted_20110302.htm. Accessed on April 7,2014.
- Kreidl KO, Kim DY, Mansour SE. Prevalence of significant intraocular sequelae in blunt orbital trauma. Am J Emerg Med. 2003;21:525-528.
- Cheung CA, Rogers-Martel M, Golas L, et al. Hospital-based ocular emergencies: epidemiology, treatment, and visual outcomes. Am J Emerg Med. 2014;32:221-224.
- Eye Injury Registry. Available at: http://eyeinjuryregistry.org/home.html. Accessed on January 19, 2014.
- Knoop KJ, Dennis WR, Hedges JR. Ophthalmologic procedures. In Clinical Procedures in Emergency Medicine. 5th ed. Edited by Roberts JR, Hedges JR, et al. Philadelphia: Saunders; 2010.
- Sharma R, Brunette DD. Ophthalmology. In Rosen's Emergency Medicine: Concepts and Clinical Practice. 7th ed. Edited by Marx JA, Hockberger RS, Walls RM, et al. St. Louis: Mosby; 2010.
- Brady SM, McMann MA, Mazzoli RA, et al. The diagnosis and management of orbital blowout fractures: update 2001. Am J Emerg Med. 2001;19:147-154.
- Harries A, Shah S, Teismann N, et al:. Ultrasound assessment of extraocular movements and papillary light reflex in ocular trauma. Am J Emerg Med. 2010;28:956-959.
- Acerra JR. Globe rupture. Available at: http://emedicine.medscape.com/article/798223-overview#a0199. Accessed on February 10, 2014.
- Peak DA. Acute orbital compartment syndrome. Available at: http://emedicine.medscape.com/article/799528-overview. Accessed on January 25, 2014.
- Blavais M. Bedside emergency department ultrasonography in the evaluation of ocular pathology. Acad Emerg Med. 2000;7:947.
- Blavais M, Theodoro D, Sierzenski PR. Clinical practice: A study of bedside ocular ultrasound in the emergency department. Acad Emerg Med. 2002;9(8):791.
- Liu Y, Chen J. Focused Bedside Ocular Ultrasound. Acad Emerg Med. 2008;15(8):792.