A 57-year-old male with unknown past medical history becomes unresponsive as witnessed by bystanders. He is found to be in PEA on arrival to the emergency department with ACLS in progress. Does the presence of cardiac activity on bedside ultrasound during ACLS correlate with improved survival of this patient?
Article
Gaspari R, Weekes A, Adhikari S, et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrests. Resuscitation. 2016;109:33-39.
Objective
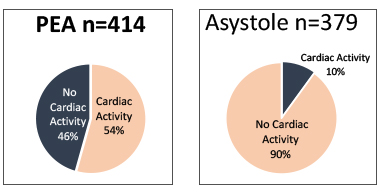
To determine whether cardiac activity on ultrasound during ACLS is associated with improved survival in patients presenting with out-of-hospital arrest or in-ED arrest with PEA or asystole. The primary outcome was survival to hospital admission. Secondary outcomes were survival to hospital discharge and ROSC.
Background
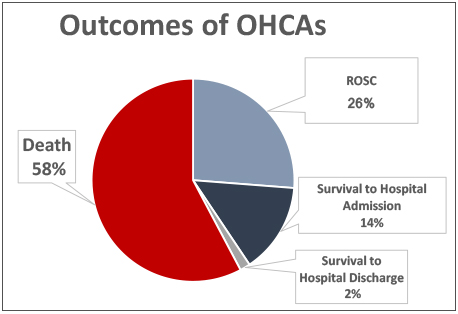
Of approximately 300,000 out-of-hospital cardiac arrests (OHCAs) annually in the U.S., more than 78% are transported to the ED. Fewer than 8% of all OHCAs survive to hospital discharge. Factors associated with survival include the presence of shockable cardiac rhythm and early defibrillation, availability of bystander CPR and ROSC in the field. POCUS can provide immediate information on cardiac activity as well as potentially identifying rapidly reversible causes of cardiac arrest such as pericardial effusion and pneumothorax. However, no large studies have been performed to explore the role of POCUS in guiding ACLS. The study is sought to determine the association between sonographically visible cardiac activity and survival for patients with PEA or asystole.
Design
- Multi center, prospective, protocol-driven observational study
- United States and Canada study sites; 1 coordinating site, 6 regional centers and 13 local sites
Inclusion criteria: non-traumatic cardiac arrest in asystole or PEA and had US imaging performed during their resuscitation
Exclusion criteria: Resuscitation not continued after initial ultrasound, resuscitation efforts discontinued due to a DNR order, resuscitation lasted < 5 minutes
Study Protocol
- POCUS at the beginning of ACLS in the ED and a second US examination at the end of resuscitation
- All ultrasounds were performed during pauses in resuscitation
- CPR was not halted to obtain US images
- Subxiphoid or parasternal long axis to identify cardiac activity by EM physicians credentialed in bedside US
Primary outcome: Survival to hospital admission
Secondary outcomes: ROSC and survival to hospital discharge
Key Results
Enrolled n=953; Included n=793
- 208 (26.2%) achieved ROSC (95% CI 23.3 – 29.4)
- 114 (14.4%) survived to hospital admission (95% CI 12.1 – 17.0)
- 13 (1.6%) survived to hospital discharge (95% CI 0.9 – 2.8)
Agreement between initial US interpretation and review was substantial (κ=0.63)
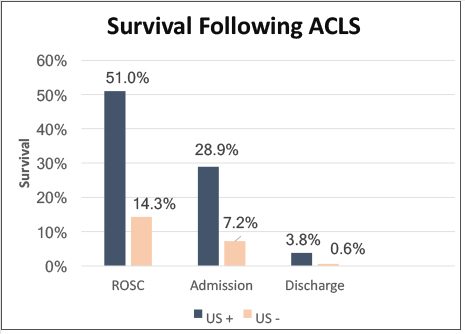
From 263 (33%) of patients with cardiac activity on initial US:
- 134 (51.0%) achieved ROSC
- 76 (28.9%) survived to hospital admission
- 10 (3.8%) survived to hospital discharge
From 530 (67%) of patients with NO cardiac activity on initial US:
- 76 (14.3%) achieved ROSC
- 38 (7.2%) survived to hospital admission
- 3 (0.6%) survived to hospital discharge
Cardiac activity on POCUS is associated with increased ROSC (OR 3; 2-4.5; p <0.0001), increased survival to hospital admission (OR 3.6; 2.2-5.9; p <0.0001) and increased survival to hospital discharge (OR 5.7; 1.5-21.9; p 0.11).
POCUS identified conditions that supported deviation from ACLS medication protocols:
Pericardial effusion 34 patients †’ attempted pericardiocentesis 13, survival to hospital discharge 2
Suspected PE 15 patient †’ thrombolysis 2, survival to hospital discharge 1
Conclusion
The presence of cardiac activity on the initial POCUS during resuscitation is the variable most associated with survival following cardiac arrest. ROSC rate was found to be over 50% if cardiac activity was detected compared to 14.1% if no cardiac activity detected. Additionally, POCUS may increase survival in OHCAs by identifying cases where non-ACLS interventions (pericardiocentesis, thrombolysis) are necessary.