A 59-year-old male presents to the emergency department in cardiac arrest. It was a witnessed arrest, and high-quality CPR was initiated almost immediately. Paramedics found him in PEA and they continued ACLS throughout a short transport to the hospital. After his fourth round of compressions and epinephrine, a palpable femoral pulse was obtained. History for the patient was extremely limited, but his son said he thought he might have diabetes and he had heard him talk about having some chest discomfort from time to time in the past. After ROSC was obtained, an EKG was completed that showed some generalized slight ST depressions but no STEMI. The patient is normotensive with a normal heart rate. Labs show a potassium of 5, magnesium of 2.4, pH of 7.25, and troponin of 2.4. After discussion with the ICU for admission and consideration for hypothermia protocol, the intensivist suggests you consult cardiology for possible catheterization.
Article
Wilson M, Grossestreuer AV, Gaieski DF, et al. Incidence of coronary intervention in cardiac arrest survivors with non-shockable initial rhythms and no evidence of ST-elevation MI (STEMI). Resuscitation. 2017;113:83-86.
Objective
To evaluate the rate of percutaneous coronary intervention (PCI) in cardiac arrest patients with a non-shockable initial rhythm who achieve return of spontaneous circulation (ROSC) and do not have evidence of STEMI on EKG
Background
Improved outcomes have been shown with early coronary angiography and intervention in arrest patients with STEMI after ROSC or ventricular fibrillation (VF)/ventricular tachycardia (VT) during arrest. Per the 2015 AHA Guidelines, it is currently a class IIa recommendation for emergent coronary angiography in patients with out-of-hospital cardiac arrest (OHCA) of suspected cardiac origin without STEMI because EKG findings in arrest patients have been shown to be poorly predictive of coronary artery occlusion. A meta-analysis showed an incidence of coronary artery disease (CAD) of 59-71% in all post-arrest patients; however, the patient population included a large number of STEMIs and VF/VT rhythms. It is generally suggested that non-shockable rhythms in arrest are more likely to be due to non-cardiac causes, and the rate of significant CAD in this patient population is not well-known.
Hypothesis
"In cardiac arrest patients with a non-shockable initial rhythm who obtain ROSC and do not have evidence of STEMI, the incidence of coronary intervention would be uncommon (<5%)."
Design
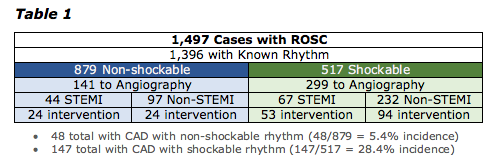
- Retrospective analysis of data from a registry of cardiac arrest patients from 18 participating institutions from January 2000 through May 2014
- All cases of cardiac arrest with known initial rhythms were identified and divided based on the rhythm and whether they underwent angiography.
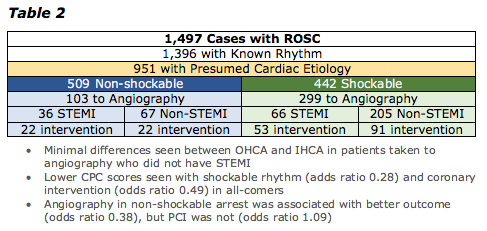
- A secondary analysis was completed on patients with a suspected cardiac etiology of the arrest, and in-hospital and out-of-hospital arrests were compared.
Inclusion criteria: Cardiac arrest as defined by loss of pulses requiring chest compressions and ROSC as defined by the presence of a pulse for at least 20 minutes
Exclusion criteria: No documented initial rhythm
Primary outcome: Incidence of CAD (determined by rate of PCI)
Secondary outcomes: Cerebral performance category (CPC) scores
Cerebral Performance Categories Scale
- CPC 1. Good cerebral performance: conscious, alert, able to work, might have mild neurologic or psychologic deficit.
- CPC 2. Moderate cerebral disability: conscious, sufficient cerebral function for independent activities of daily life. Able to work in sheltered environment.
- CPC 3. Severe cerebral disability: conscious, dependent on others for daily support because of impaired brain function. Ranges from ambulatory state to severe dementia or paralysis.
- CPC 4. Coma or vegetative state: any degree of coma without the presence of all brain death criteria. Unawareness, even if appears awake (vegetative state) without interaction with environment; may have spontaneous eye opening and sleep/awake cycles. Cerebral unresponsiveness.
- CPC 5. Brain death: apnea, areflexia, EEG silence, etc.
Results
Authors' Conclusion and Limitations
- There is an unexpectedly high incidence of PCI in patients taken for angiography who had an initial non-shockable rhythm and no STEMI on EKG (24.7%).
Relationship between the CAD that was found and the arrest itself is unclear.
- Overall incidence of 5.4% in non-shockable rhythms is higher than expected, and rate of 8.6%when including only those with suspected cardiac cause shows that we are not able to predict who will benefit and who will not.
- Randomization to catheterization after arrest may help identify who exactly will benefit and who will not.
- Retrospective study in population with unknown prevalence means detection of CAD cannot be used to determine causation of arrest or be compared to other populations.
- Decision to proceed with angiography introduced bias as shown by the fact that going to angiography improved outcomes in non-shockable rhythms but intervention did not.
Our Conclusions and Applications for the ED
- At first glance, the rate of coronary lesions requiring intervention of 5.4% in patients with arrest and non-shockable rhythms is impressive.
- However, the clinical significance of these lesions is completely unknown and this data must be interpreted cautiously.
- This caution is particularly appreciated when noting that patients who underwent angiography and did not receive intervention had better CPC scores than those who received intervention.
- This data does confirm the idea that patients with cardiac arrest and shockable rhythms or STEMI on EKG do frequently benefit from catheterization and this should become standard of care.
- If clinical suspicion is very high for a cardiac cause of arrest after achieving ROSC and no STEMI is seen on EKG, it may be reasonable to consult cardiology for possible catheterization, but ED Cath Lab activation should not be standard practice.



